Testing for Chagas Cardiac Disease at a Large Safety-net Hospital in New England
Alyse Wheelock, MD
Authors:
Alyse Wheelock, MD1, Sukhmeet Sandhu, MD1, Alyssa Loskill, BA2, Rachel Marcus, MD5, Deepa Gopal, MD6, Davidson. H. Hamer, MD3,4, Natasha Hochberg, MD, MPH3
- Internal Medicine Residency Program, Department of Medicine, Boston Medical Center, Boston, MA
- Boston University School of Public Health, Boston, MA
- Department of Global Health, Boston University School of Public Health, Boston, MA
- Section of Infectious Diseases, Department of Medicine, Boston University School of Medicine, Boston, MA
- MedStar Union Memorial Hospital, Baltimore, MD, United States; Latin American Society of Chagas
- Department of Medicine, Cardiovascular Division, Boston University Medical Center, Boston, MA
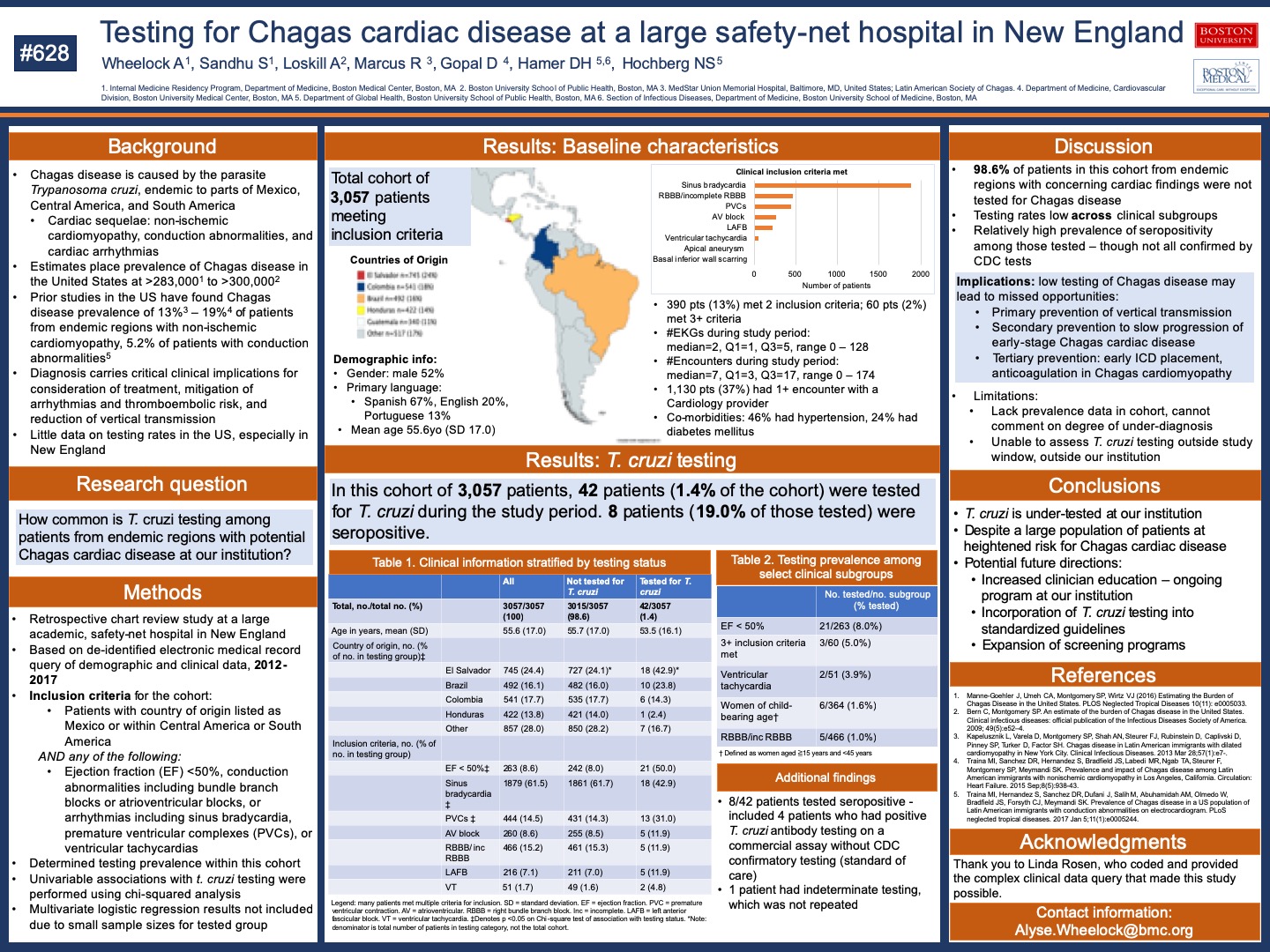
Prior research suggests that Chagas disease, caused by the parasite Trypanosoma cruzi, is an important etiology of non-ischemic cardiomyopathy and cardiac arrhythmias among people who originate from Mexico, Central America, and South America. Less than 1% of the estimated 300,000 people living with Chagas disease in the United States have been diagnosed and treated, however. This study aims to determine the frequency of Chagas disease testing among individuals from endemic regions who display signs suggestive of Chagas heart disease. Retrospective chart review was performed of electronic medical records from 2012-2017 at an academic safety net hospital in Boston. Inclusion criteria were patients born in Mexico, Central America, and South America found to have ejection fraction (EF) <50%, conduction abnormalities (including bundle branch blocks or atrioventricular blocks), or arrhythmias (including sinus bradycardia, premature ventricular complexes, or ventricular tachycardias). Data on demographics, electrocardiograms (EKG), echocardiography, Chagas disease diagnostics, and treatment were collected. Descriptive statistics were performed. 3,057 patients’ records were pulled from a electronic medical records query based on the inclusion criteria. The most frequent countries of origin in the final cohort were El Salvador (n=745), Colombia (n=541) and Brazil (n=492). Sinus bradycardia was the most common inclusion criterion met (1,879/3,057 patients, or 61.5%), followed by right bundle branch block (466/3,057 patients, or 15.2%) and premature ventricular complexes (444/3,057 patients, or 14.5%). 450/3,057 patients (14.7%) met two or more criteria for inclusion. 263/3,057 patients (8.6%) were included due to EF <50%. Only 42/3,057 (1.4%) patients had Chagas serologies ordered during the study duration. Of these patients, 8/42 (19.0%) had any positive test for Chagas disease, 33/42 (78.6%) had negative testing, and 1/42 (2.4%) had indeterminate results. Patients who were tested for Chagas disease were more likely to have an EF <50% (p = <0.001) and more likely to meet more than one inclusion criterion (p = <0.001). Among the subgroup of 263 patients with EF <50%, 21 patients (8.0%) had testing for Chagas disease. 60 patients met three or more inclusion criteria, and among this supgroup, 3 patients (5%) had Chagas disease testing. Rates of Chagas disease testing were very low among this cohort of patients from endemic countries with EKG and echocardiographic findings potentially consistent with Chagas cardiac complications. Among those patients tested, a significant proportion tested positive. The initial findings of our study suggest a need to expand diagnosis and treatment of Chagas cardiac disease among Latin American immigrants in North America.
7 comments
Great work, Alyse – clearly points to the need of action at our institution, and likely generalizable well beyond our walls. I like the research question and results sections being highlighted as well, and good use of figures.
Nice work! And welcome to BMC/BU ID
Alyse, great work! Really interesting and important findings! These findings certainly support the expansion of testing for CD in the at risk cohort you identified. It will be important for us to develop an intervention plan to accomplish this goal! Well-done!
Dave
Wow, interesting project and finding — especially since patients had 7 encounters on average. I wonder if an epic alert could be built to highlight people who meet criteria for testing. Thanks for taking on this project!
Highlights the importance of a careful history about geographic origin and awareness of the entity. I recommend a medical grand rounds on the subject and findings of this study – perhaps a combined clinical/research MGRs in the new academic year. David
Great work! I am surprised by how little we screen even in those with low EF. This highlights how we should be screening more.
wow, interesting! What’s your best guess as to the number of missed diagnoses, downstream implications of those missed diagnoses, cost-benefit analysis for more expansive screening? nice job.!