Research Week 2022 – Sarah Olofsson, MD
Category: Education
A New Model for Teaching Primary Palliative Care on the Inpatient Renal Service
Authors: Sarah Olofsson, Aala Jaberi, Perla Macip-Rodriguez
Background: Palliative care is an essential part of residency training, however many residents do not feel adequately equipped to engage in these conversations on subspecialty services when they may feel patients’ disease states are beyond their expertise. As the value of palliative care services are becoming increasingly recognized and there are growing shortages in the palliative care trained workforce, many physician organizations are recognizing the need to train other frontline providers on how to begin these conversations (a phenomenon termed “primary palliative care”). This project proposes a method for reviewing primary palliative care concepts with subspecialty attendings who can then teach these topics to residents who rotate through their service.
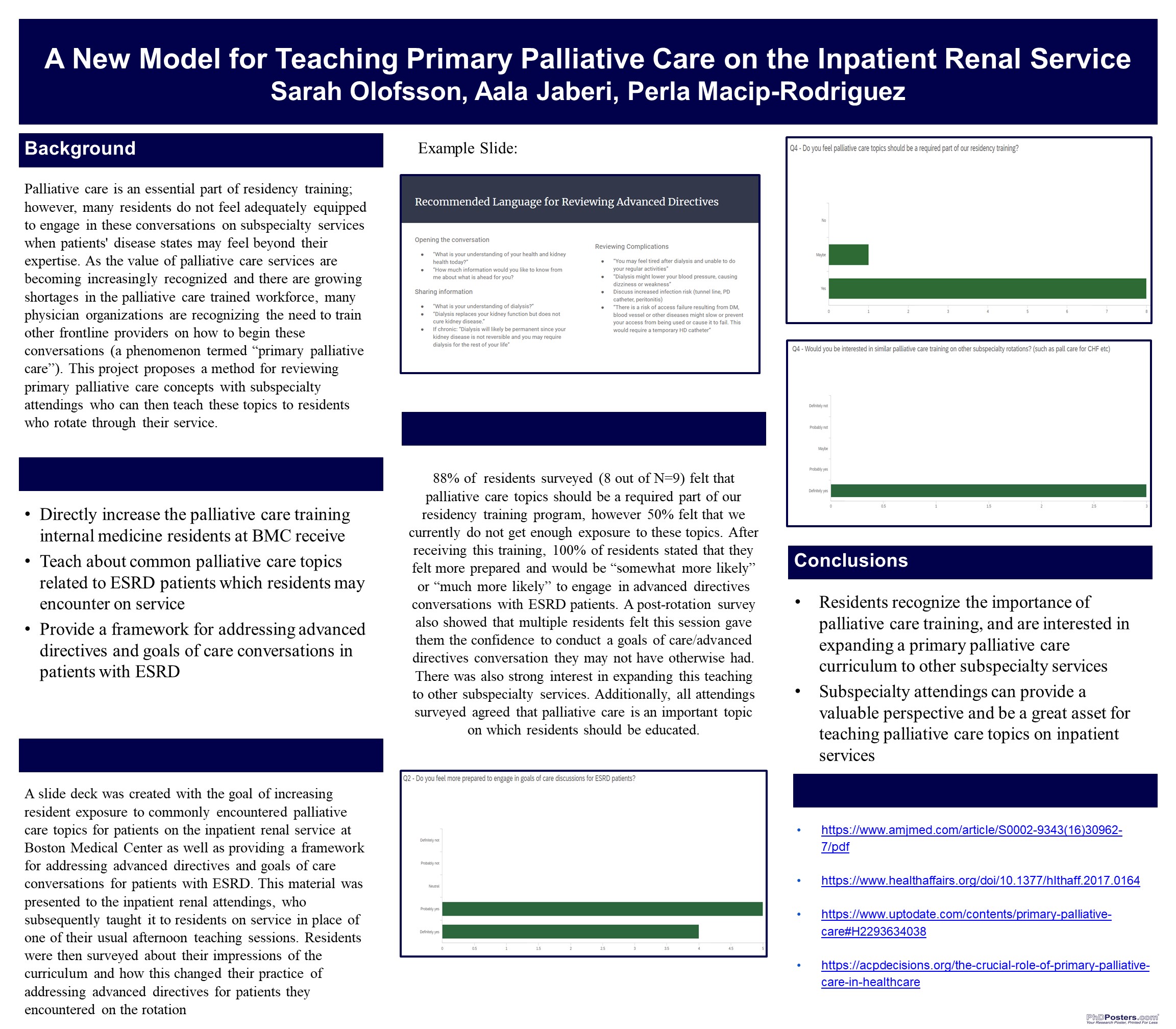
Methods: A slide deck was created with the goal of increasing resident exposure to commonly encountered palliative care topics for patients on the inpatient renal service at Boston Medical Center as well as providing a framework for addressing advanced directives and goals of care conversations for patients with ESRD. This material was presented to the inpatient renal attendings, who subsequently taught it to residents on service in place of one of their usual afternoon teaching sessions. Residents were then surveyed about their impressions of the curriculum and how this changed their practice of addressing advanced directives for patients they encountered on the rotation
Results: All residents surveyed felt that palliative care topics should be a required part of our residency training program, however 50% felt that we currently do not get enough exposure to these topics. After receiving this training, 100% of residents surveyed stated that they felt more prepared and would be “somewhat more likely” or “much more likely” to engage in advanced directives conversations with ESRD patients. A post-rotation survey also showed that multiple residents felt this session gave them the confidence to conduct a goals of care/advanced directives conversation they may not have otherwise had. There was also strong interest in expanding this teaching to other subspecialty services. Additionally, all attendings surveyed agreed that palliative care is an important topic on which residents should be educated.
Conclusions
-Residents recognize the importance of palliative care training, and are interested in expanding a primary palliative care curriculum to other subspecialty services
-Subspecialty attendings can provide a valuable perspective and be a great asset for teaching palliative care topics on inpatient services
References
https://www.amjmed.com/article/S0002-9343(16)30962-7/pdf
https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0164
https://www.uptodate.com/contents/primary-palliative-care#H2293634038
https://acpdecisions.org/the-crucial-role-of-primary-palliative-care-in-healthcare