Research Week 2022 – Rebecca Burns, MD
Title: Comparing COVID-19-related Morbidity and Mortality between Patients with and without
Substance Use: A Retrospective Cohort Study
Rebecca Burns MDc*, Angela McLaughlin MDa-b* MPHTM, Morgan Ryan MSd, Pranay Sinha MDa-b, Wafaa Abbasi BSe, Jacqueline Hicks, PhDd, Sabrina Assoumou MD, MPHa-b,
*Contributed equally to the project
- Section of Infectious Diseases, Department of Medicine, Boston Medical Center, Boston, Massachusetts, USA 20119
- Section of Infectious Diseases, Department of Medicine, Boston University School of Medicine, Boston, Massachusetts, USA 02119
- Section of Internal Medicine, Boston University School of Medicine, Boston, Massachusetts, USA 02119
- Department of Biostatistics, Boston University School of Public Health, Boston, Massachusetts, USA 02119
- Boston University School of Medicine, Boston, Massachusetts, USA 02119
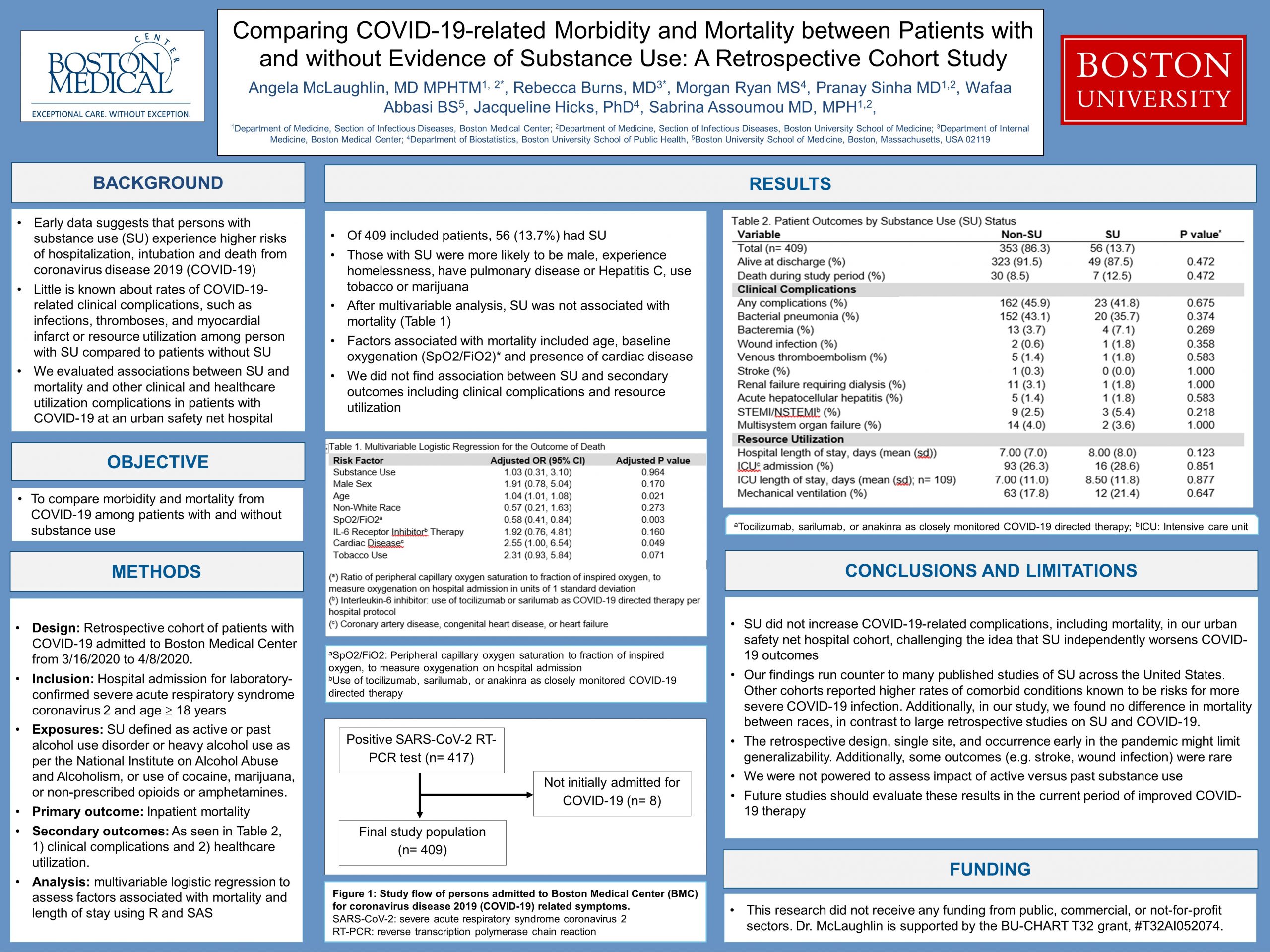
Introduction: The coronavirus 2019 (COVID-19) pandemic has emphasized and contributed to the unique healthcare barriers faced by individuals with substance use (SU), such as stigma, housing insecurity and limited preventative care. Early research suggested that substance use experience higher risk of hospitalization, intubation, and death from coronavirus disease 2019 (COVID-19), although recent data has been mixed. Few studies have considered how COVID-19 might impact incidence of other clinical complications or resource utilization in this group. We compared morbidity and mortality among individuals with and without known SU who were admitted to an urban safety net hospital for COVID-19 infections.
Methods: We performed a retrospective cohort study of patients 18 years or older who were admitted to Boston Medical Center (BMC) with COVID-19. Infection was defined as a positive reserve-transcriptase polymerase chain reaction test (nasopharyngeal or tracheal aspirate). The study ran from March 16th to April 8th, 2020, at which time the hospital’s COVID-19 treatment protocol was revised. We excluded patients admitted for reasons other than COVID-19 and those who contracted COVID-19 during admission. Substance use was defined as current or past alcohol use disorder or heavy alcohol use (as defined by the National Institute on Alcohol Abuse and Alcoholism); use of cocaine; use of non-prescribed opioids, benzodiazepines, or amphetamines. Substances such as hallucinogens and inhalants were not excluded as they rarely appeared in chart review. Marijuana and tobacco use were not defined as SU.
The primary outcome was inpatient mortality. Secondary outcomes were clinical complications (secondary bacterial infections, renal failure requiring dialysis, venous thromboembolism, stroke, hepatitis, myocardial infarct, multisystem organ failure) and resource utilization (mechanical ventilation, ICU admission, hospital and ICU length of stay, and time to ICU admission and intubation). We used multivariable regression to assess the relationship between SU and mortality.
Results: A total of 409 patients were included with 56 (13.7%) meeting criteria for SU. The mean age was 56 years, the majority were from racial/ethnic groups previously reported to have a higher proportion of severe COVID-19 (including 50% Black and 20% Hispanic/Latino). Those with evidence of SU were more likely to be male, have experienced homelessness, have pulmonary disease or hepatitis C, or use tobacco or marijuana. Otherwise, demographics, including mean age and racial/ethnic backgrounds were similar between the groups. After multivariable analysis controlling for age, sex, non-white race, baseline oxygenation by SpO2/FiO2, administration of IL-6 receptor inhibitor therapy, cardiac disease, and tobacco use, SU was not associated with mortality (aOR 1.03; 95% CI, 0.31-3.10). Factors significantly associated with mortality included age (aOR 1.04; 1.01-1.08), baseline oxygenation by SpO2/FiO2 (aOR 0.58; 0.41-0.84), and presence of cardiac disease (aOR 2.55; 1.00-6.54). Likewise, we did not find any association between SU and either secondary clinical complications or healthcare utilization.
Conclusions: In this group of patients at urban safety net hospital, rates of morbidity and mortality were similar between those with and without SU. This suggests that previously reported outcomes of increased COVID-19 complications may in fact reflect higher rates of comorbid conditions among those with SU rather than an independent association with substance use itself.