Research Week 2022 – Munizay Paracha, MD
Title: Understanding Mortality Among Hematology Oncology Patients Identified From Hospital Administrative Data
Authors: Munizay Paracha, MD1, Anish Parekh, MD, MPH1, Ayesha Sheikh, MD2, Stanley Nwabudike, MD3, Tsion Fikre, Naomi Ko, MD, MPH1
- Boston University Medical Center, Department of Hematology/Oncology, 2. Saint Vincent Medical Group, Massachusetts, 3. Presbyterian Cancer Care, New Mexico
Abstract
Background
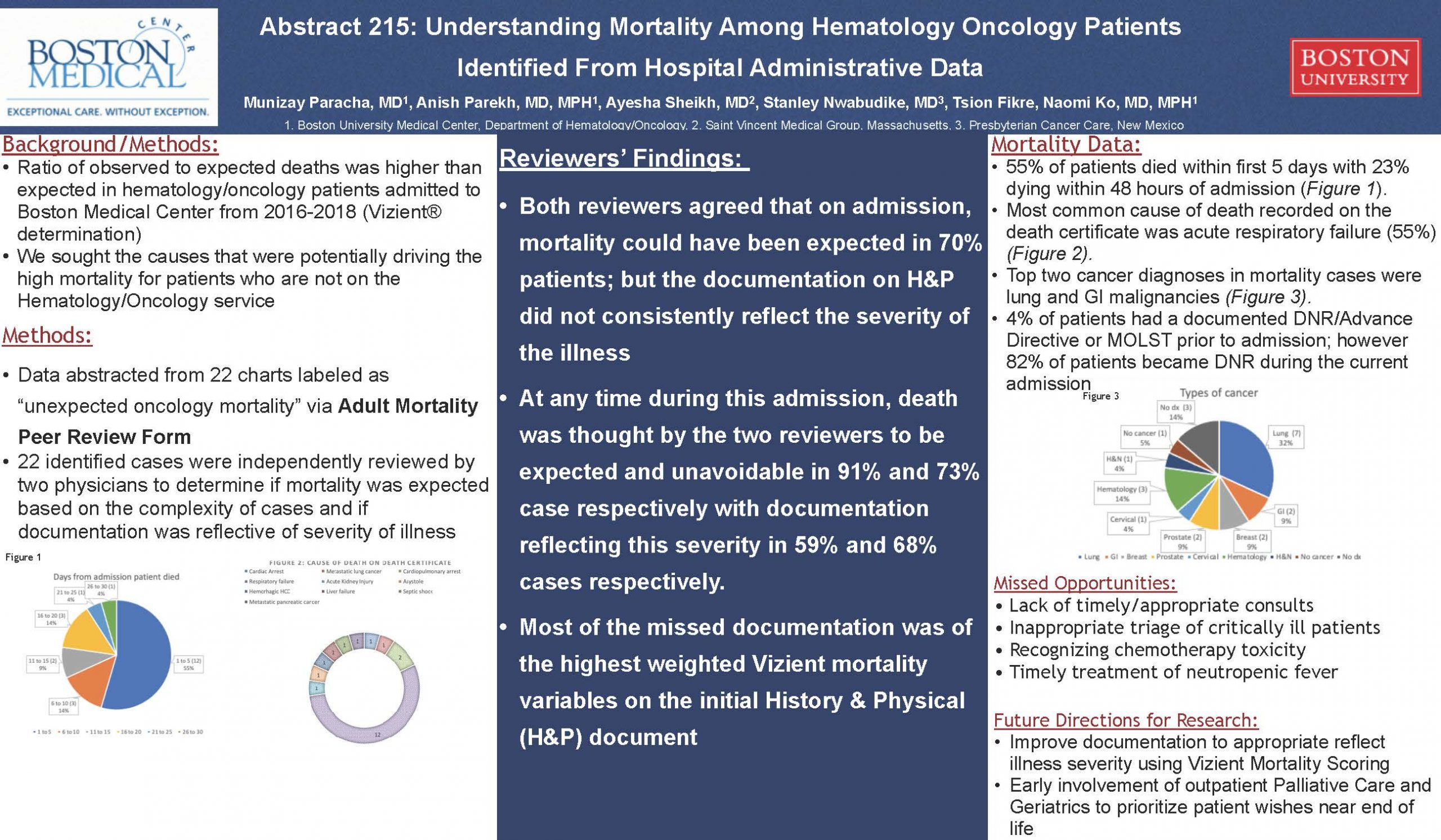
Hospital administrative data has large ramifications for quality of care and quality improvement projects. Unexpected inpatient mortality among patients with a hematology/oncology (H/O) diagnostic related group (DRG) is not widely studied and reported. We sought to investigate the unexpected inpatient mortality rate among cancer patients who were admitted to a large, urban, tertiary care safety net teaching hospital.
Methods
We obtained the hospital’s adjusted mortality rate and evaluated the subset of specific observed/expected deaths ratio (O/E) of patients with a primary H/O diagnosis. We chart reviewed each case that was identified as an unexpected mortality which occurred at the hospital from 2016 to 2018. A chart abstraction tool was designed for data abstraction. Data elements included demographics, location of admission, comorbid conditions, if mortality was expected, if documentation was reflective of the severity of the illness. Two independent reviewers abstracted each chart. Every case was discussed with a third reviewer to make a final determination regarding if mortality was expected based on the complexity of case and if documentation was reflective of severity of illness.
Results
On review of the inpatient mortality data, the O/E for the H/O diagnostic related group (DRG) from Vizient® was 1.14. Twenty two cases were identified as having an unexpected death. Among those cases, 23% of patients were transferred from an outside hospital, and 23% of patients did not have a known cancer diagnosis at the time of admission. In the majority of cases, documentation on admission did not accurately reflect severity of illness, specialists in hematology or oncology were not consulted at time of diagnosis. We noted the majority of patients were not followed by a hematologist/oncologist within the hospital system (63.6%). In 55% of patients, the cause of death was acute respiratory failure, and 14% of patients had an Advance Directive/DNAR in the chart prior to admission. Delayed antibiotics in febrile neutropenia and a missed blood transfusion reaction were causes of unexpected deaths.
Conclusions
Hospital generated data reported that mortality among H/O patients was greater than projected, however careful chart review of each case demonstrated a significant number of cases that were expected but the severity of illness was not documented properly to account for the death. Templates for proper documentation using the Vizient mortality variables is a key area to lower unexpected inpatient mortality.