Research Week 2022 – Matthew Custodio, MD
Title: Provider perceptions of fresh frozen plasma transfusion in variceal bleeding lag behind current evidence and vary across clinical specialties
Authors: Matthew J. Custodio1, Kelly E. Diaz2, Sartajdeep S. Kahlon3, Andrew Canakis4, Stephen H. Caldwell2, Christine Reardon5, Jordan Spector6, Pramod K. Guru7, Reggie Thomasson8, Michael F. Harrison9, Eric W. Chak3, Nathalie Urrunaga4, Zachary Fricker10, Jonathan G. Stine11, Arpan Mohanty1
1Section of Gastroenterology, Boston Medical Center, Boston University School of Medicine,
Boston, MA, USA.
2Division of Gastroenterology and Hepatology, University of Virginia Medical Center, Charlottesville, VA, USA
3Department of Internal Medicine, UC Davis Medical Center, Sacramento, CA, USA
4Division of Gastroenterology and Hepatology, University of Maryland School of Medicine, Baltimore, MD, USA
5Division of Pulmonary and Critical Care, Boston University School of Medicine, Boston, MA, USA
6Department of Emergency Medicine, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA
7Departmentof Critical Care Medicine, Mayo Clinic, Jacksonville, FL, USA
8Department of Pathology and Laboratory Medicine, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA.
9Department of Emergency Medicine, Mayo Clinic, Jacksonville, FL, USA
10Division of Gastroenterology/Liver Center, Beth Israel Deaconess Medical Center, Boston, MA, USA
11Division of Gastroenterology & Hepatology, Department of Medicine, Pennsylvania State University Milton S. Hershey Medical Center, PA, USA
Background and Aims: Fresh frozen plasma (FFP) transfusion in cirrhosis has little effect on coagulation parameters and is potentially harmful in patients with variceal bleeding. However, its use in patients with cirrhosis and variceal bleeding is common. We hypothesized that FFP transfusion practice lags behind available evidence and guidance as providers perceive FFP transfusion to be beneficial or harmless. Since patients with variceal bleeding are co-managed by gastroenterology (GI), critical care medicine (CCM) and emergency medicine (EM) providers, we hypothesized that provider perceptions of FFP transfusion vary across specialties. This study aims to assess and compare provider perceptions of FFP transfusion in variceal bleeding in GI, CCM and EM providers.
Method: We developed, validated, and administered a self-reported, anonymous, electronic survey to GI, CCM and EM providers in 4 academic, tertiary care centers in USA. Providers who had taken care of at least one patient with bleeding varices in the last year were eligible. We compared Likert scale responses to questions on FFP transfusion practices of GI and EM/CCM providers using the Mann-Whitney test.
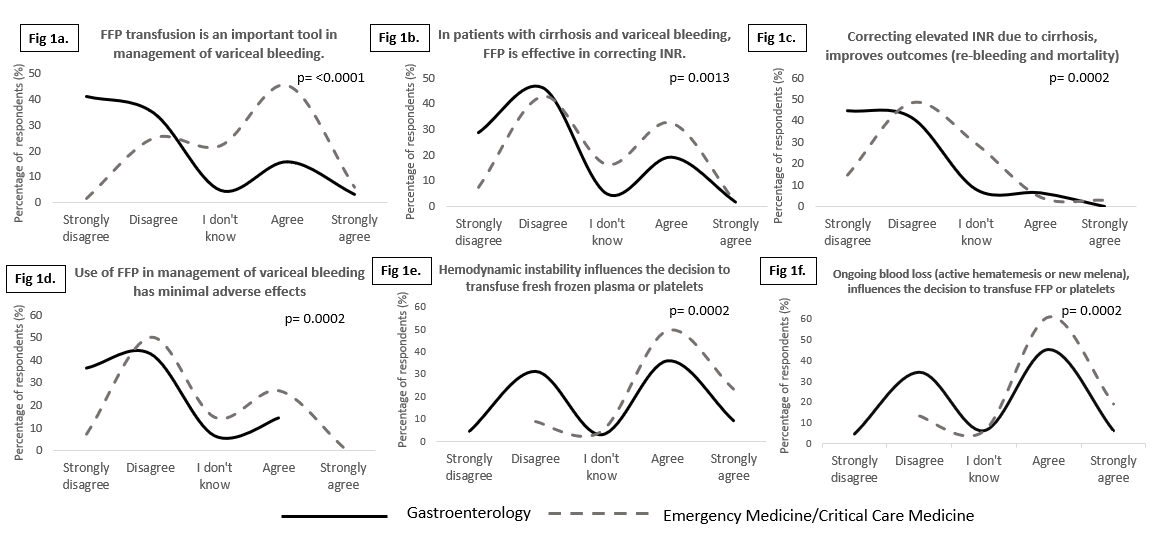
Results: The survey was deployed to 115 GI, 201 CCM and 308 EM providers. We received 64 GI (55%), 31 CCM (22%) and 38 EM (20%) valid responses. As compared to EM/CCM providers (27%), most GI providers (76%) disagreed with the statement FFP was an important tool in management of variceal bleeding (Fig 1a). Only 22% GI and 32% EM/CCM providers felt that FFP was effective in correcting INR (Fig 1b). More GI providers (75%) disagreed with the statement INR improves variceal bleeding outcomes as compared to EM/CCM (50%) providers (Fig 1c). Most providers disagreed with the statement FFP use in variceal bleeding has minimal side effects (86% GI, 63% EM/CCM, Fig 1d). More GI providers felt that hemodynamic instability (36%) or ongoing blood loss (39%) did not warrant FFP transfusions as compared to EM/CCM providers (Fig 1e/1f). Most providers (73%) did not think that medical liability was a factor in the decision making on blood product transfusions in variceal bleeding.
Conclusion: There are substantial differences in provider perceptions of the utility of FFP transfusions in patients with variceal bleeding in frontline specialties despite recent advances in available evidence. Even with a small sample size, we note significant variations in provider perceptions between specialties. Multi-specialty society guidelines and hospital-wide transfusion guidelines may help translate currently available evidence into clinical practice across all specialties in this complex patient population.
Figures: