Research Week 2022 – Joshua Gilman, MD
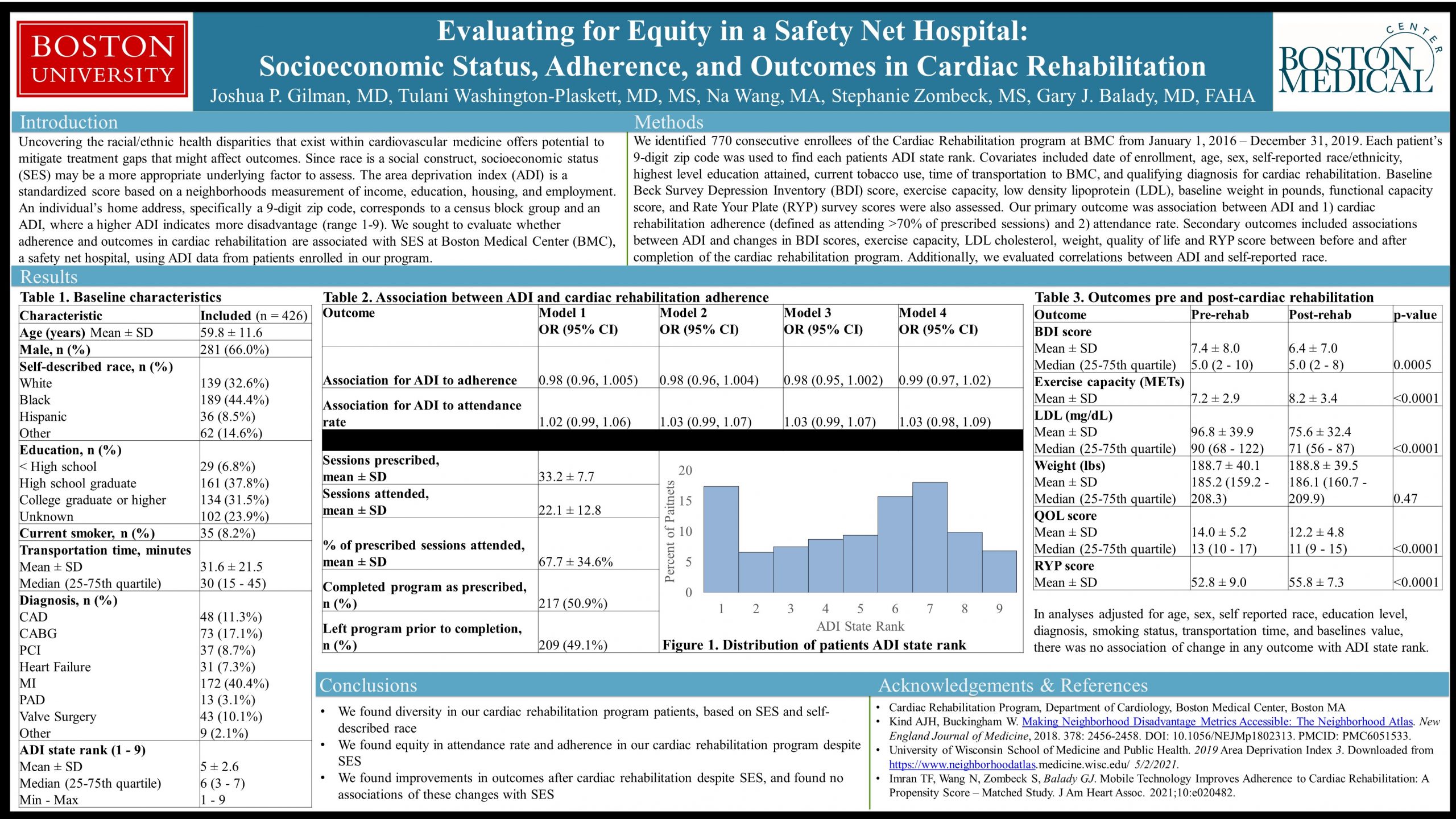
Evaluating for Equity in a Safety Net Hospital: Socioeconomic Status, Adherence, and Outcomes in Cardiac Rehabilitation
Joshua P. Gilman, MD, Tulani Washington-Plaskett, MD, MS, Na Wang, MA, Stephanie Zombeck, MS, Gary J. Balady, MD, FAHA
Uncovering the racial/ethnic health disparities that exist within cardiovascular medicine offers potential to mitigate treatment gaps that might affect outcomes. Since race is a social construct, socioeconomic status (SES) may be a more appropriate underlying factor to assess. We sought to evaluate whether adherence and outcomes in cardiac rehabilitation are associated with SES in a safety net hospital. The area depravation index (ADI) reflects income, education, employment, and housing quality within a given 9-digit zip, where a higher ADI indicates more disadvantage (range 1-10). Home ADI’s were obtained for 770 enrollees of the Cardiac Rehabilitation Program at Boston Medical Center from 2016-2020. Associations between ADI and adherence (attending >70% of sessions) was evaluated while controlling for age, sex, race, education, diagnosis, smoking and transport times. Secondary outcomes included associations of ADI with change in exercise capacity, LDL, weight, quality of life, nutrition, and depression scores. Among the enrollees, 197 had missing covariates and 147 did not have a zip code with an associated ADI, leaving 426 patients for analysis. Enrollees had a mean age of 59.8 years, 34% were female, 44% self-reported as black and 9% as Hispanic. The ADI for patients varied (mean 5; median 6). The primary outcome after adjustment revealed no association for ADI with adherence (OR, 1.03 95% CI: 0.99-1.07) or attendance rate (OR, 0.98 95% CI: 0.96-1.004). Secondary outcomes improved among patients regardless of ADI. In our safety net hospital that provides care without exception, we found equity in cardiac rehabilitation program outcomes despite SES.
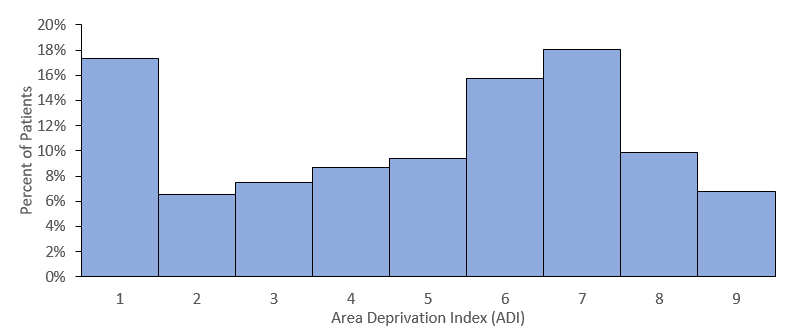
Figure 1. Distribution of included patients’ ADI state rank.