Research Week 2022 – Jennifer Bayly, MD & Emily Lupez, MD
TITLE: Primary care and telemedicine utilization in patients with type 2 diabetes at a safety-net hospital before and after onset of the COVID-19 pandemic
Lupez, Emily*; Bayly, Jennifer*, Xuan, Ziming, Lasser, Karen E.
*Authors contributed equally
BACKGROUND: During the COVID-19 pandemic, healthcare systems implemented telemedicine to ensure safe uninterrupted care for patients who require regular follow up such as those with type 2 diabetes (T2DM). While studies have documented disparities in access to telemedicine, few have compared overall changes in primary care utilization pre and post pandemic, and few have focused on disparities in utilization among patients with T2DM in safety-net settings.
METHODS: We conducted a retrospective analysis of electronic health record data of all established adult primary care patients with T2DM at the largest safety-net hospital in New England. We defined a minimum of semiannual visits as standard of care (SOC). Logistic regression models analyzed primary care utilization during pre-pandemic (3/15/18-3/14/20) and post-pandemic onset (3/15/20-3/15/21) time periods according to patient demographics, insurance, and visit type (in-person, telemedicine-all, phone, video), adjusting for comorbidity and A1c.
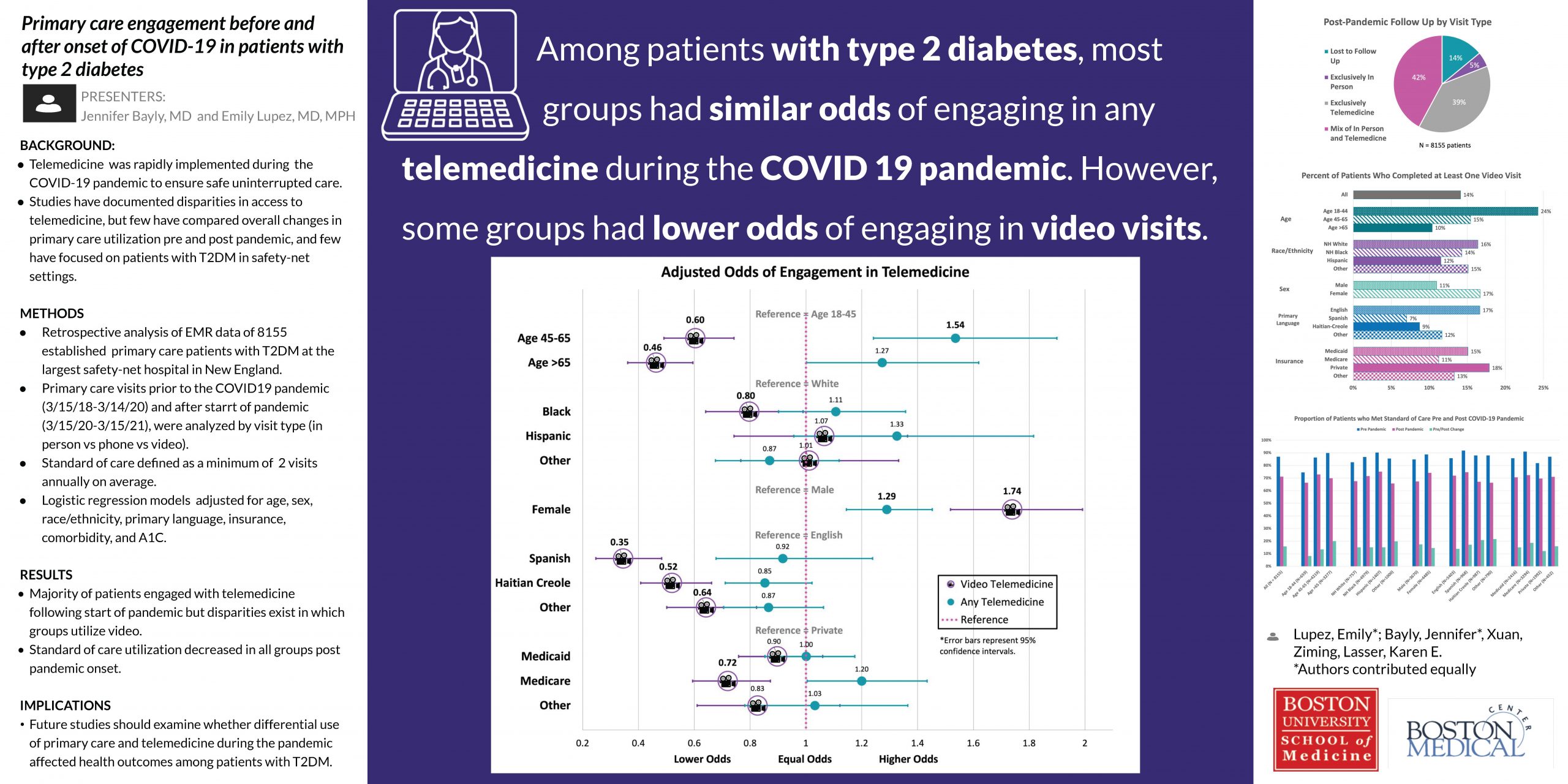
RESULTS: Of 8155 patients with T2DM, 86% had at least one primary care visit after pandemic onset. Of those patients, 5.8% had exclusively in-person visits, 45.2% had exclusively telemedicine visits, and 49.0% had a mix of both. Of 30,094 post-pandemic visits, 78% were telemedicine (88.1% via phone, 7.3% via video, and 4.6% unknown type). Pre-pandemic, 87% of patients had SOC utilization, and patients who are non-white, female (vs. male), Spanish speaking (vs. English), age >44, and have Medicare or Medicaid (vs. commercial) had higher odds of SOC utilization. Post-pandemic onset, 71% of patients had SOC utilization, and patients who are Hispanic (vs. white), female (vs. male), age 45-65, and have Medicare had higher odds of SOC utilization. Females (vs. males) and 45-65 year-olds (vs 18-44) had higher odds of engaging in at least one telemedicine visit (OR [95%CI]: female 1.3 [1.1-1.5]; 45-65 1.5 [1.2-1.9]). Patients who are Black (vs. white), non-English speaking, age >44, and with Medicare had lower odds of completing at least one video visit (OR [95%CI]: Black 0.8 [0.6-0.99]; Spanish 0.3 [0.2-0.5], Haitian-Creole 0.5 [0.4-0.7]; 45-65 0.6 [0.5-0.7], >65 0.5 [0.4-0.6]; Medicare 0.7 [0.6-0.9]), while females (vs. males) had higher odds (OR [95%CI]: 1.7 [1.5-2.0]).
CONCLUSIONS: Most patients with T2DM had primary care visits at least semiannually prior to the pandemic. Following the pandemic, this proportion decreased across all groups. Odds of having visits at least semiannually were different according to demographics, insurance, and pandemic time-period. Most post-pandemic visits were via telemedicine, few of which included video. Odds of engagement in telemedicine did not differ between patients of different race/ethnicity, language, and insurance status. However, Black patients, older patients, and those who do not speak English are less likely to use video. Future studies should examine whether differential use of primary care and telemedicine during the pandemic has affected T2DM outcomes.
LEARNING OBJECTIVE
#1: Identify how patients with Type 2 Diabetes utilized primary care prior to and during the COVID-19 pandemic.
#2: Describe how patient demographics and insurance status impact primary care and telemedicine utilization among patients with Type 2 Diabetes.