Research Week 2022 – Devin Driscoll, MD
Category: Scientific Clinical Research
Project Title: “Why Does My Knee Hurt After I Got My Knee Replaced?”: Evaluation of Neuropathic-like Symptoms and Objective Signs of Neuropathy Post-Knee Replacement in Patients with Knee Osteoarthritis
Authors: Devin Driscoll, Priyanka Ballal, Na Wang, Laura Frey-Law, James Torner, Michael Nevitt, Tuhina Neogi
Abstract
Background:
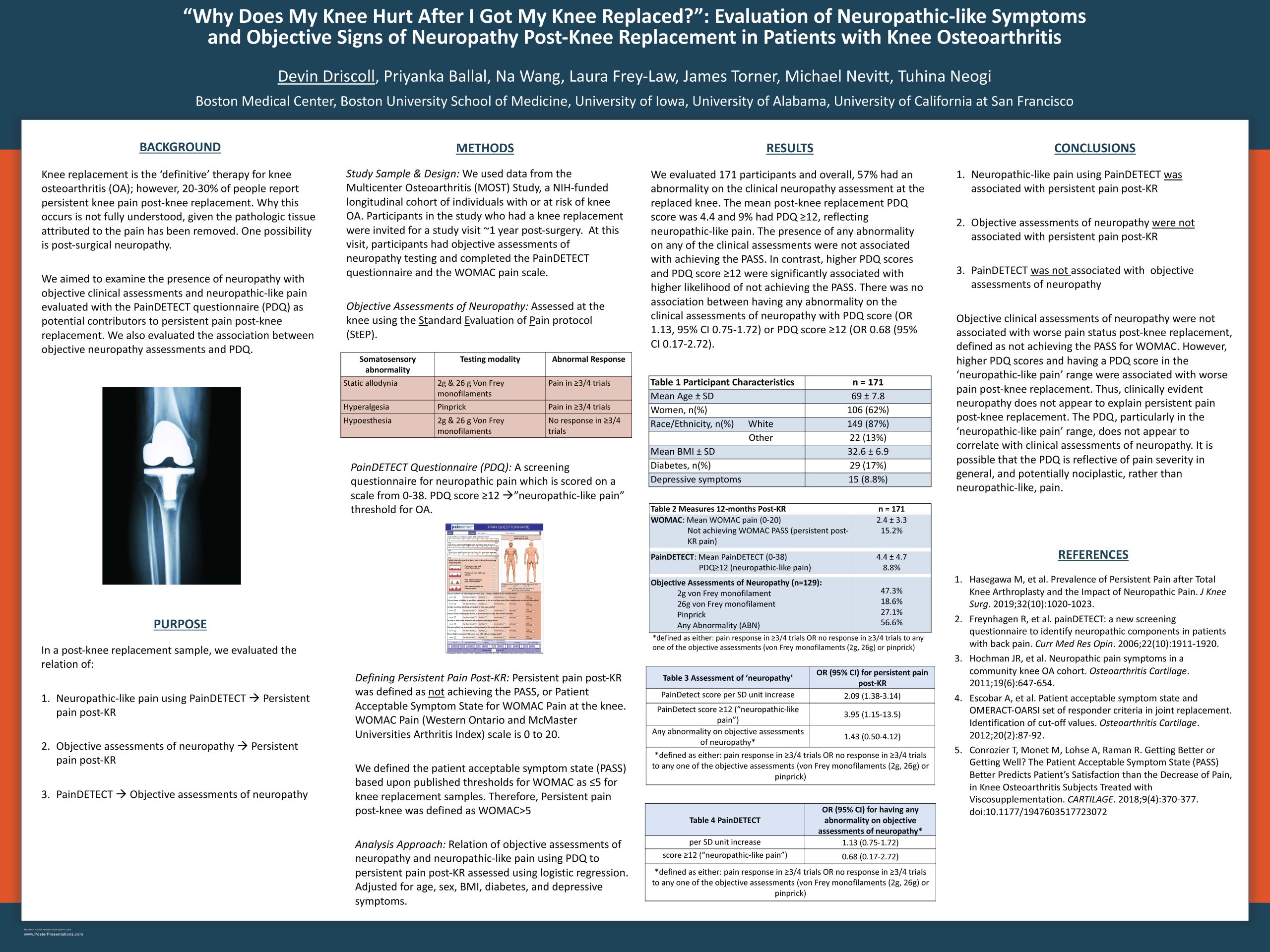
Some people with knee osteoarthritis (OA) have persistent pain post-knee replacement, but why this occurs is not fully understood. One possibility is post-surgical neuropathy. We aimed to examine presence of neuropathy with objective clinical assessments and neuropathic-like pain evaluated with the PainDETECT questionnaire (PDQ) as potential contributors to persistent pain post-knee replacement. We also evaluated the association between objective neuropathy assessments and PDQ.
Methods:
We used data from the Multicenter Osteoarthritis (MOST) Study, a NIH-funded longitudinal cohort of individuals with or at risk of knee OA. Participants in the study who had a knee replacement were invited for a study visit ~1 year post-surgery. We obtained clinical assessments for neuropathy at that time. We also obtained the PDQ and WOMAC (0-20). We defined the patient acceptable symptom state (PASS) based upon published thresholds for WOMAC as 5/20 for knee replacement samples. A PDQ score of ≥12 was considered neuropathic-like. We evaluated the relation of the clinical neuropathy assessments and the PDQ to achievement of the PASS post-knee replacement, using logistic regression, adjusting for potential confounders.
Results:
We evaluated 171 participants and overall, 57% had an abnormality on the clinical neuropathy assessment at the replaced knee. The mean post-knee replacement PDQ score was 4.4 and 9% had PDQ ≥12, reflecting neuropathic-like pain. The presence of any abnormality on any of the clinical assessments were not associated with achieving the PASS. In contrast, higher PDQ scores and PDQ score ≥12 were significantly associated with higher likelihood of not achieving the PASS. There was no association between having any abnormality on the clinical assessments of neuropathy with PDQ score (OR 1.13, 95% CI 0.75-1.72) or PDQ score ≥12 (OR 0.68 (95% CI 0.17-2.72).
Conclusion:
Objective clinical assessments of neuropathy were not associated with worse pain status post-knee replacement, defined as not achieving the PASS for WOMAC. However, higher PDQ scores and having a PDQ score in the ‘neuropathic-like pain’ range were associated with worse pain post-knee replacement. Thus, clinically evident neuropathy does not appear to explain persistent pain post-knee replacement. The PDQ, particularly in the ‘neuropathic-like pain’ range, does not appear to correlate with clinical assessments of neuropathy. It is possible that the PDQ is reflective of pain severity in general, and potentially nociplastic, rather than neuropathic-like, pain.