Research Week 2022 – Colin Pierce, MD
Colin Pierce
SRAD Abstract – Clinical Vignette
Background
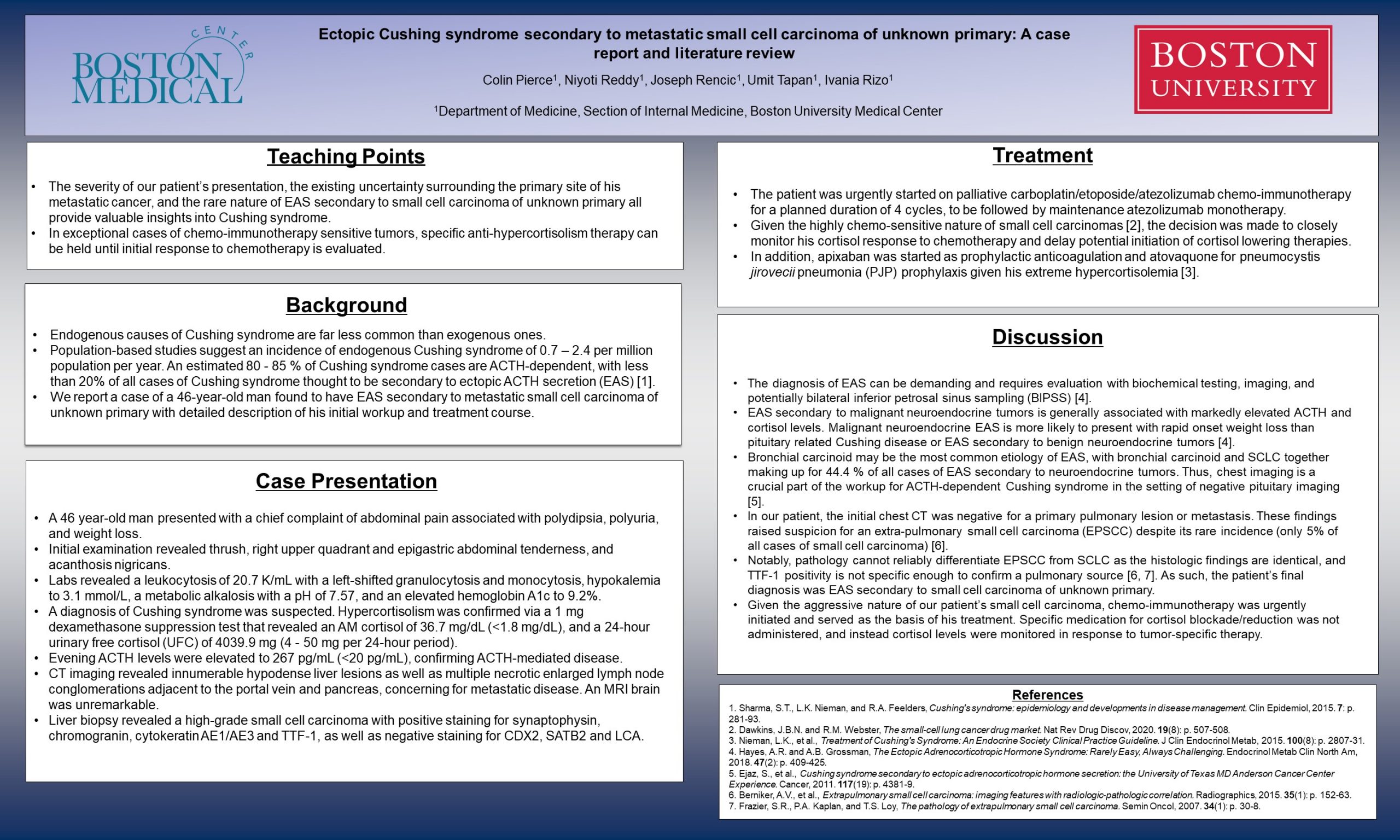
Cushing syndrome results from prolonged exposure to supra-physiologic glucocorticoid levels. Endogenous causes of Cushing syndrome are far less common than exogenous ones. Population-based studies suggest an incidence of endogenous Cushing syndrome of 0.7 – 2.4 per million population per year. An estimated 80 – 85 % of Cushing syndrome cases are ACTH-dependent, with less than 20% of all cases of Cushing syndrome thought to be secondary to ectopic ACTH secretion (EAS) [1]. We report a case of a 46-year-old man found to have EAS secondary to metastatic small cell carcinoma of unknown primary with detailed description of his presenting history, initial workup, and treatment course.
Case presentation
A 46 year-old man presented with a chief complaint of abdominal pain associated with polydipsia, polyuria, severe fatigue, and a 40-pound weight loss. Initial examination revealed thrush, right upper quadrant and epigastric abdominal tenderness, and acanthosis nigricans. He was afebrile, tachycardic to the low 100s, and hypertensive to 154/108. He had Class I obesity with a BMI of 33 and increased abdominal waist circumference. Initial labs were notable for a leukocytosis of 20.7 K/mL with a left-shifted granulocytosis and monocytosis, hypokalemia to 3.1 mmol/L, and a metabolic alkalosis with a pH of 7.57. He had an elevated hemoglobin A1c (HbA1c) to 9.2%.
A diagnosis of Cushing syndrome was suspected. Hypercortisolism was confirmed via a 1 mg dexamethasone suppression test that revealed an AM cortisol of 36.7 mg/dL (<1.8 mg/dL), and a 24-hour urinary free cortisol (UFC) of 4039.9 mg (4 – 50 mg per 24-hour period). Evening ACTH levels were elevated to 267 pg/mL (<20 pg/mL), confirming ACTH-mediated disease.
CT chest, abdomen and pelvis imaging revealed innumerable hypodense liver lesions as well as multiple necrotic enlarged lymph node conglomerations adjacent to the portal vein and pancreas, concerning for metastatic disease. There were no pulmonary lesions. An MRI brain was unremarkable. Liver biopsy revealed a high-grade small cell carcinoma with positive staining for synaptophysin, chromogranin, cytokeratin AE1/AE3 and TTF-1, as well as negative staining for CDX2, SATB2 and LCA.
Treatment
Chemotherapy was urgently initiated in the setting of metastatic small cell carcinoma. The patient was started on palliative carboplatin/etoposide/atezolizumab chemo-immunotherapy for a planned duration of 4 cycles to be followed by maintenance atezolizumab monotherapy. Given the highly chemo-sensitive nature of small cell carcinomas [2], we made the decision to closely monitor his cortisol response to chemotherapy and delay potential initiation of cortisol lowering therapies such as metyrapone. The patient was also started on apixaban for prophylactic anticoagulation and atovaquone for pneumocystis jirovecii pneumonia (PJP) prophylaxis given his extreme hypercortisolemia [3].
Discussion
EAS can occur secondary to benign or malignant neuroendocrine tumors. The diagnosis of EAS can be demanding and requires evaluation with biochemical testing, imaging studies, and potentially bilateral inferior petrosal sinus sampling (BIPSS), all of which have caveats and should be interpreted within the appropriate clinical context [4]. EAS secondary to malignant neuroendocrine tumors is generally associated with markedly elevated ACTH and cortisol levels, although there is an overlap with levels seen in Cushing disease. Notably, malignant neuroendocrine EAS is more likely to present with rapid onset weight loss and catabolic features than pituitary related Cushing disease or EAS secondary to benign neuroendocrine tumors [4]. Furthermore, mineralocorticoid effects (e.g., hypokalemia, metabolic alkalosis) and hyperpigmentation are more often present in the setting of EAS aggressive malignancies [4].
Small cell lung carcinoma (SCLC) is traditionally thought to be the most common of the neuroendocrine tumors associated with EAS with an estimated incidence of up to 50% of all cases in one review of the literature [5]. However, a recent retrospective analysis suggests that bronchial carcinoid may in fact be a more common etiology of the syndrome, with bronchial carcinoid and SCLC together making up for 44.4 % of all cases of EAS secondary to neuroendocrine tumors. Thus, chest imaging is a crucial part of the workup for ACTH-dependent Cushing syndrome in the setting of negative pituitary imaging [6]. In our patient, the initial chest CT was negative for a primary pulmonary lesion or metastasis; subsequent PET imaging also failed to localize a primary intrathoracic lesion. These findings, in conjunction with our patient’s status as a non-smoker, raised suspicion for an extra-pulmonary small cell carcinoma (EPSCC) despite its rare incidence (only 5% of all cases of small cell carcinoma) [7].
Notably, pathology cannot reliably differentiate EPSCC from SCLC as the histologic findings are identical, and TTF-1 positivity, while more common in pulmonary than extra-pulmonary small cell carcinomas, is not specific enough to confirm a pulmonary source [7, 8]. As such, the patient’s final diagnosis was EAS secondary to small cell carcinoma of unknown primary.
Given the aggressive and metastatic nature of our patient’s small cell carcinoma, chemo-immunotherapy was urgently initiated and served as the basis of his treatment. Specific medication for cortisol blockade/reduction was not administered, and instead cortisol levels were monitored in response to tumor-specific therapy. Six weeks later, after completion of 2 cycles of chemo-immunotherapy, the tumor burden decreased with an associated dramatic drop in 24-hour UFC levels from >4000 mg to 5.9 mg per 24-hour period, along with an improvement in glycemic control.
Learning points
- The florid nature of our patient’s presentation, the existing uncertainty surrounding the primary site of his metastatic cancer, and the rare nature of EAS secondary to small cell carcinoma of unknown primary all provide valuable insights into Cushing syndrome.
- In exceptional cases of chemo-immunotherapy sensitive tumors, specific anti-hypercortisolism therapy can be held until initial response to chemotherapy is evaluated.
Sources
- Sharma, S.T., L.K. Nieman, and R.A. Feelders, Cushing’s syndrome: epidemiology and developments in disease management. Clin Epidemiol, 2015. 7: p. 281-93.
- Dawkins, J.B.N. and R.M. Webster, The small-cell lung cancer drug market. Nat Rev Drug Discov, 2020. 19(8): p. 507-508.
- Nieman, L.K., et al., Treatment of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab, 2015. 100(8): p. 2807-31.
- Hayes, A.R. and A.B. Grossman, The Ectopic Adrenocorticotropic Hormone Syndrome: Rarely Easy, Always Challenging. Endocrinol Metab Clin North Am, 2018. 47(2): p. 409-425.
- Elston, M.S., et al., Severe Cushing’s syndrome due to small cell prostate carcinoma: a case and review of literature. Endocr Connect, 2017. 6(5): p. R80-R86.
- Ejaz, S., et al., Cushing syndrome secondary to ectopic adrenocorticotropic hormone secretion: the University of Texas MD Anderson Cancer Center Experience. Cancer, 2011. 117(19): p. 4381-9.
- Berniker, A.V., et al., Extrapulmonary small cell carcinoma: imaging features with radiologic-pathologic correlation. Radiographics, 2015. 35(1): p. 152-63.
- Frazier, S.R., P.A. Kaplan, and T.S. Loy, The pathology of extrapulmonary small cell carcinoma. Semin Oncol, 2007. 34(1): p. 30-8.