Research Week 2022 – Alan Chan, MD
TITLE: Evaluating neuroborreliosis in immunocompromised hosts
AUTHOR: Alan Chan, MD
INSTITUTIONS (ALL):
- Internal Medicine, Boston Medical Center, Boston, MA, United States.
ABSTRACT BODY:
Learning Objective 1: Recognize the hallmarks of each stage of Lyme disease
Learning Objective 2: Identifying early and late neurologic manifestations of Lyme disease in immune competent and compromised hosts
Learning Objective 3: Treat central nervous system Lyme disease with appropriate parental and oral antibiotics
Case:
A 71 year-old-male with past medical history of IBS, inflammatory polyarthritis on abatacept and methotrexate presented for nausea, vomiting, and diarrhea. On the day of discharge, he was noted to have Bell’s Palsy. He endorsed recent tick exposure and Lyme EIA was IgM positive and IgG negative. He later presented to his primary care provider where he endorsed headache, left facial droop, inability to close left eyelid, and left-lower extremity weakness. Due to concern for neuroborreliosis (CNS Lyme), he was admitted for an expedited work-up. Lumbar puncture showed WBC 25 (85% lymphs), RBC 6, protein 77, glucose 62. A meningitis PCR panel was negative. He was started on intravenous ceftriaxone and subsequently switched to oral doxycycline to complete in the outpatient setting. On his follow-up visit, he had improved facial weakness with near resolution of prior symptoms.
Discussion:
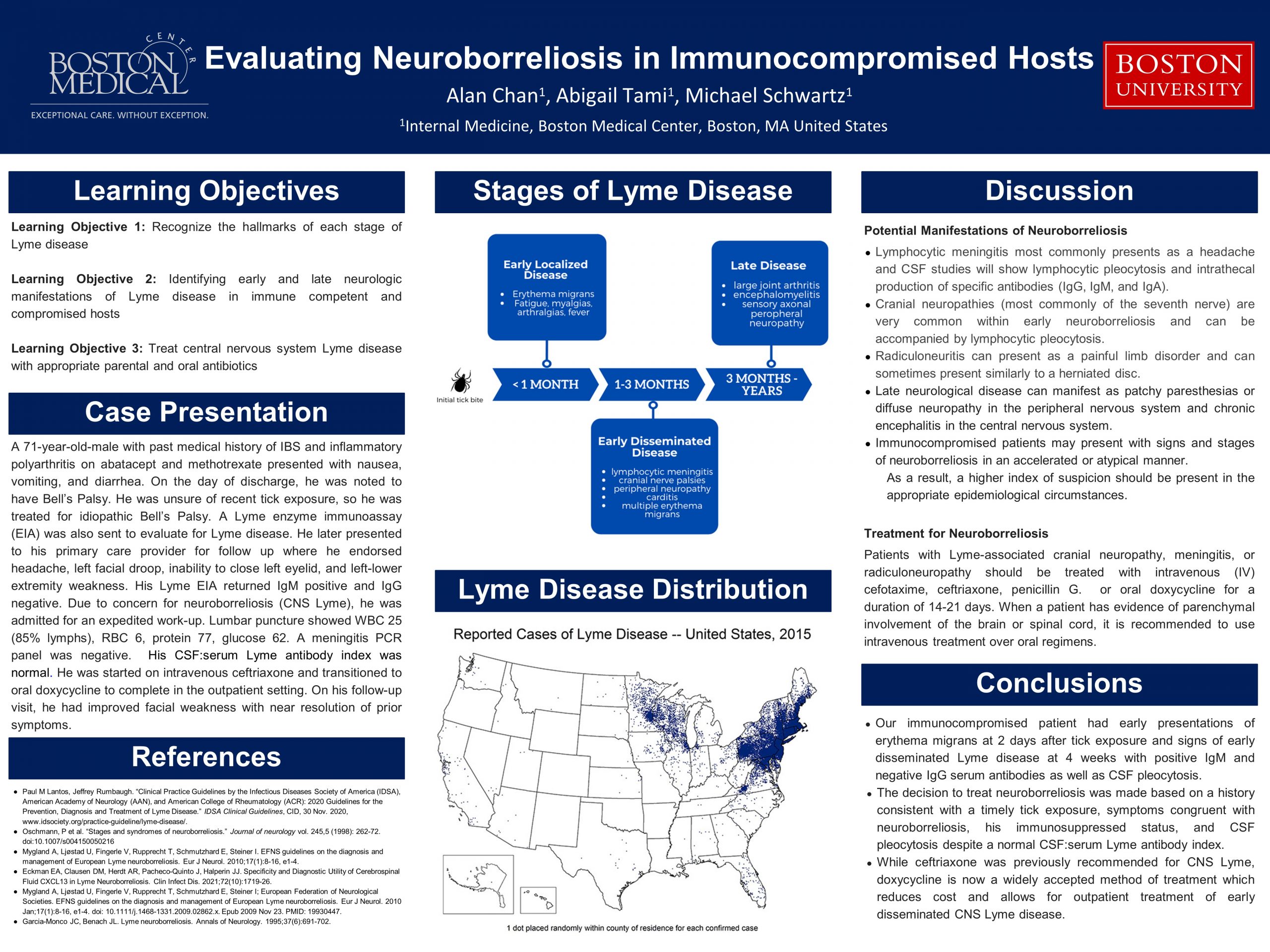
The clinical manifestations of Lyme disease are fractionated into three stages based on time from exposure: early localized (days to one month), early disseminated (>6 weeks to months), and late disease (months to years). Neurological manifestations of Lyme disease can occur at early or late disseminated stages and can involve the central and peripheral nervous systems. Early localized disease is exemplified by erythema migrans with symptoms of fatigue, headache, arthralgias, and myalgias. Early disseminated disease can manifest as facial nerve palsy, lymphocytic meningitis, peripheral neuropathy, and carditis. Late neurological disease can manifest as patchy paresthesias or diffuse neuropathy in the peripheral nervous system and chronic encephalitis in the central nervous system. Immunocompromised patients may present with signs and stages of neuroborreliosis in an accelerated or atypical manner. As a result, a higher index of suspicion should be present in the appropriate epidemiological circumstances. Patients with Lyme-associated cranial neuropathy, radiculoneuropathy, or meningitis should be treated with intravenous (IV) ceftriaxone, cefotaxime, penicillin G, or oral doxycycline for a duration of 14-21 days. When a patient has evidence of parenchymal involvement of the brain or spinal cord, it is recommended to use intravenous treatment over oral regimens.
Conclusion:
Our patient had early presentations of erythema migrans at 2 days after tick exposure and signs of early disseminated Lyme disease at 4 weeks with positive IgM and negative IgG serum antibodies as well as CSF pleocytosis. The decision to treat neuroborreliosis was made based on a history consistent with a timely tick exposure, symptoms congruent with neuroborreliosis, his immunosuppressed status, and CSF pleocytosis. Lastly, while previous treatment recommendations for CNS Lyme was ceftriaxone, doxycycline is now a widely accepted method of treatment which reduces cost and allows for outpatient treatment of early disseminated CNS Lyme disease.