Acute Pancreatitis as a Rare Side Effect of Empagliflozin
Erica Saunders, MD
Case Presentation:
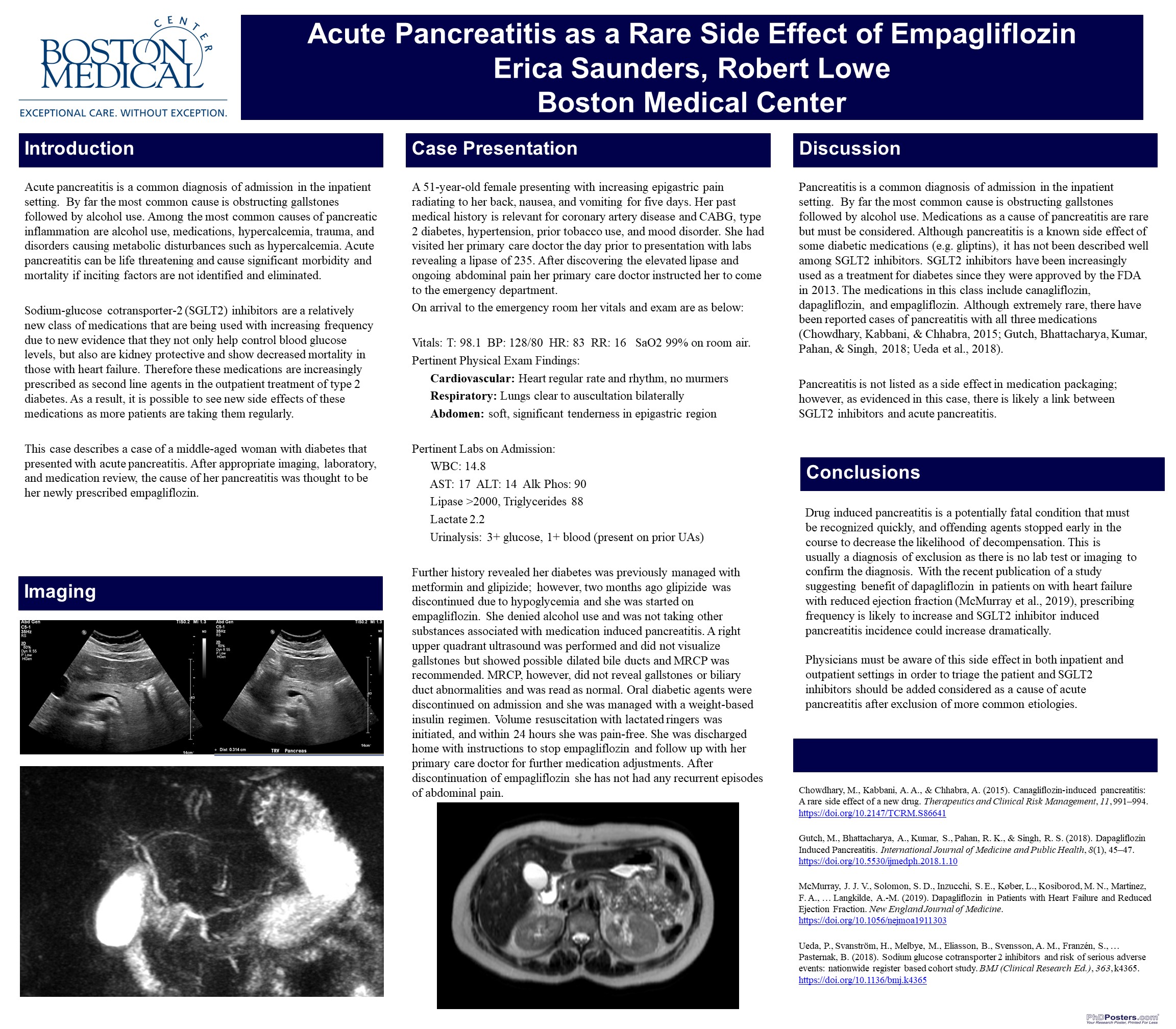
A 51-year-old female presenting with increasing epigastric pain radiating to her back, nausea, and vomiting for five days. Her past medical history is relevant for coronary artery disease and CABG, Type 2 diabetes, hypertension, prior tobacco use, and mood disorder. She had visited her primary care doctor the day prior to presentation with labs revealing a lipase of 235. On arrival to the emergency room she was afebrile, blood pressure 128/80, heart rate of 83, and oxygen saturation of 99% on room air. Her labs were notable for WBC of 14.8, normal liver enzymes, normal triglycerides, and lipase had increased to greater than 2000. Further history revealed her diabetes was previously managed with metformin and glipizide; however, two months ago glipizide was discontinued due to hypoglycemia and she was started on empagliflozin. She denied alcohol use and was not takings other substances associated with medication induced pancreatitis. A right upper quadrant ultrasound was performed and did not visualize gallstones but showed possible dilated bile ducts and MRCP was recommended. MRCP, however, did not reveal gallstones or biliary duct abnormalities and was read as normal. Oral diabetic agents were discontinued on admission and she was managed with a weight-based insulin regimen. Volume resuscitation with lactated ringers was initiated, and within 24 hours she was pain-free. She was discharged home with instructions to stop empagliflozin and follow up with her primary care doctor for further medication adjustments. After discontinuation of empagliflozin she has not had any recurrent episodes of abdominal pain.
Discussion:
Pancreatitis is a common diagnosis of admission in the inpatient setting. By far the most common cause is obstructing gallstones followed by alcohol use. Medications as a cause of pancreatitis are rare but must be considered. Although pancreatitis is a known side effect of some diabetic medications (e.g. gliptins), it has not been described well among sodium glucose cotransporter-2 (SGLT2) inhibitors. SGLT2 inhibitors have been increasingly used as a treatment for diabetes since they were approved by the FDA in 2013. The medications in this class include canagliflozin, dapagliflozin, and empagliflozin. Although extremely rare, there have been reported cases of pancreatitis with all three medications(Chowdhary, Kabbani, & Chhabra, 2015; Gutch, Bhattacharya, Kumar, Pahan, & Singh, 2018; Ueda et al., 2018). Pancreatitis is not listed as a side effect in medication packaging; however, the FDA is currently investigating a link between SGLT2 inhibitors and pancreatitis. Further studies will need to be done to determine mechanism causing pancreatic inflammation, possible underlying predisposing conditions, and reinitiating SGLT2 inhibitors after developing pancreatitis.
Conclusions:
Drug induced pancreatitis is a potentially fatal condition that must be recognized quickly, and offending agents stopped early in the course to decrease the likelihood of decompensation. This is usually a diagnosis of exclusion as there is no lab test or imaging to confirm the diagnosis. With the recent publication of a study suggesting benefit of dapagliflozin in patients on with heart failure with reduced ejection fraction(McMurray et al., 2019), prescribing frequency is likely to increase and SGLT2 inhibitor induced pancreatitis incidence could increase dramatically. Physicians must be aware of this side effect in both inpatient and outpatient settings in order to triage the patient and SGLT2 inhibitors should be added considered as a cause of acute pancreatitis after exclusion of more common etiologies.
References:
Chowdhary, M., Kabbani, A. A., & Chhabra, A. (2015). Canagliflozin-induced pancreatitis: A rare side effect of a new drug. Therapeutics and Clinical Risk Management, 11, 991–994. https://doi.org/10.2147/TCRM.S86641
Gutch, M., Bhattacharya, A., Kumar, S., Pahan, R. K., & Singh, R. S. (2018). Dapagliflozin Induced Pancreatitis. International Journal of Medicine and Public Health, 8(1), 45–47. https://doi.org/10.5530/ijmedph.2018.1.10
McMurray, J. J. V., Solomon, S. D., Inzucchi, S. E., Køber, L., Kosiborod, M. N., Martinez, F. A., … Langkilde, A.-M. (2019). Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. New England Journal of Medicine. https://doi.org/10.1056/nejmoa1911303
Ueda, P., Svanström, H., Melbye, M., Eliasson, B., Svensson, A. M., Franzén, S., … Pasternak, B. (2018). Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: nationwide register based cohort study. BMJ (Clinical Research Ed.), 363, k4365. https://doi.org/10.1136/bmj.k4365
4 comments
Erica, this is a wonderful example of the use of a Case Report to identify a potentially serious complication of an increasingly used medication. Very nicely done! Dave
Thank you for the case Erica. We nephrologists are increasingly using SGLT2i for renal protection and knowing this important side effect is very helpful.
nice job and a reminder for us to be vigilant as we increasingly use these agents
Very helpeful case report..
Tow cases of acute pancreatitis can be discovered early after canagliflozin prescribed..