Cervical Cancer, A Rare Cause of a Leukemia Reaction
Jennifer Maccarone, MD
Learning Objective 1: Recognize cervical cancer as an uncommon cause of a severe leukemoid reaction
Learning Objective 2: Develop a framework for the differential diagnosis of hyperleukocytosis
Case Presentation:
A 40-year-old African American woman with metastatic cervical cancer diagnosed April 2019 but lost to follow up presents with leukocytosis to 140,000.
At her initial re-presentation in July 2019, she was found to have leukocytosis to 40,000. CT abdomen/pelvis showed diffuse metastasis likely from a primary cervical cancer. PET revealed hypermetabolic pelvic mass with diffuse lymphadenopathy (pelvic, retroperitoneal, supraclavicular) and invasion of left iliopsoas muscle. Additionally, there was diffuse intense metabolic activity throughout the axial and appendicular skeleton that is not common with cervical cancer, raising concern for lymphoproliferative disorder, bone marrow replacement or bony metastasis. Smear showed no blasts, thus leukocytosis was felt to be likely leukemoid and paraneoplastic in the setting of locally advanced malignancy. The diffuse bone activity was felt to be due to IV dextran so no bone marrow biopsy was done.
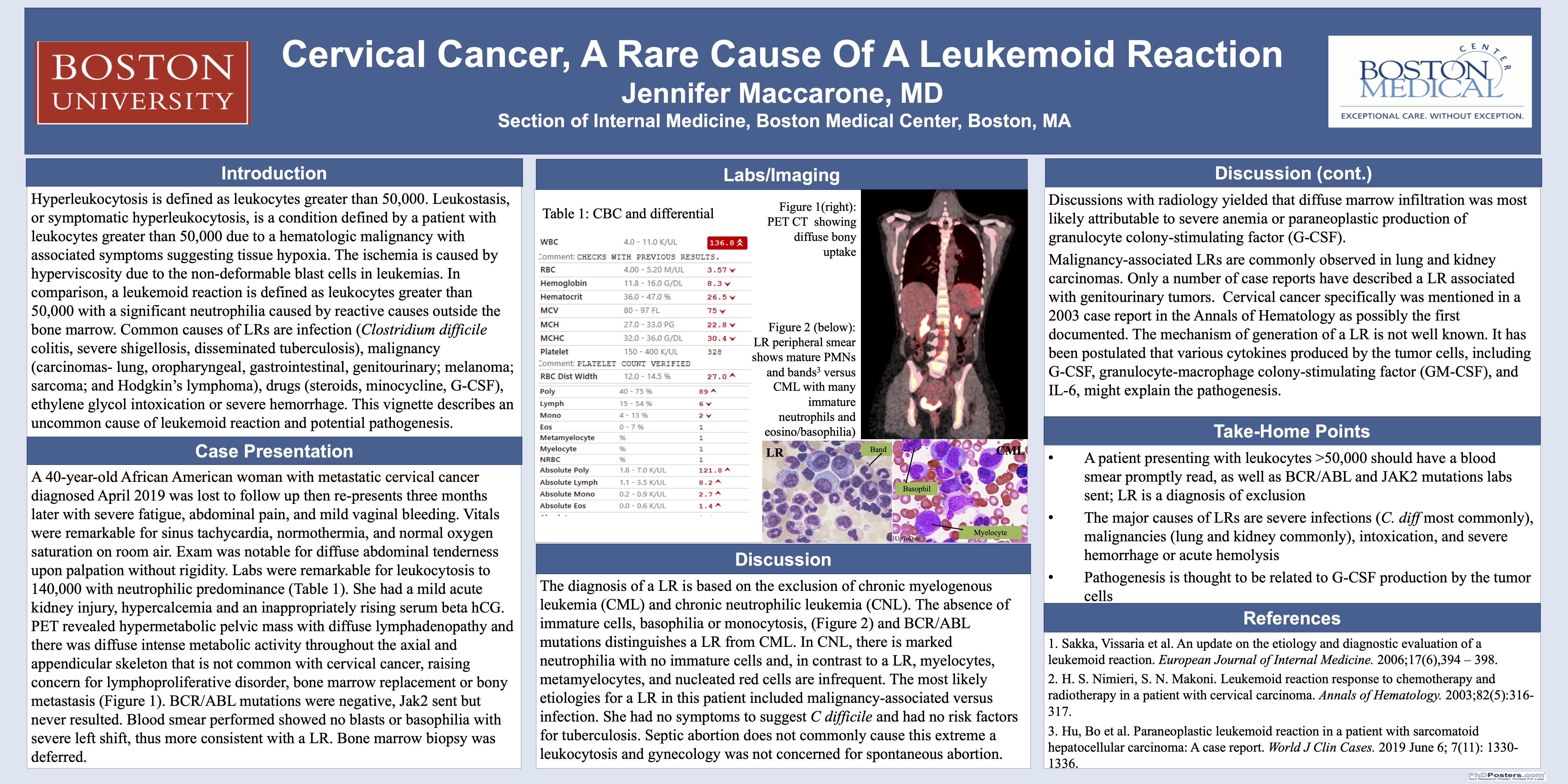
Two weeks later, the patient presented with severe fatigue, abdominal pain, and continued mild vaginal bleeding. Vitals were remarkable for sinus tachycardia, normothermia, and normal oxygen saturation on room air. Exam was notable for diffuse abdominal tenderness upon palpation without rigidity. Labs were remarkable for leukocytosis to 140,000 with 95% neutrophils, 2% bands and 3% lymphocytes. She had a mild acute kidney injury, hypercalcemia and an inappropriately rising serum beta hCG concerning for abnormal pregnancy. CT abdomen/pelvis with contrast revealed pelvic mass with diffuse worsening metastasis but no signs of pyelonephritis, colitis, or bowel obstruction. CT pulmonary angiogram showed bilateral pleural effusions with no evidence of loculations and no lung field consolidations.
Still her leukocytosis was thought to be consistent with a leukemoid reaction (LR), but the severity of hyperleukocytosis necessitated rule out of myeloproliferative disorders. BCR/ABL mutations and Jak2 mutations were sent. Discussions with radiology yielded that diffuse marrow infiltration was most likely attributable to severe anemia or paraneoplastic production of granulocyte colony-stimulating factor (G-CSF). However, hematologic malignancy could not be ruled out. Blood smear performed showed no blasts or dysmorphic cells, thus more consistent with a LR. Bone marrow biopsy was deferred.
BCR/ABL mutations were negative; Jak2 has not yet resulted. Patient received a course of carboplatin and paclitaxel, and three days later her leukocytosis began to resolve.
Discussion:
Hyperleukocytosis is defined as leukocytes greater than 50,000. Leukostasis, or symptomatic hyperleukocytosis, is a condition defined by a patient with leukocytes greater than 50,000 due to a hematologic malignancy with associated symptoms suggesting tissue hypoxia. The ischemia is caused by hyperviscosity due to the non-deformable blast cells in leukemias. In comparison, a leukemoid reaction is defined as leukocytes greater than 50,000 with a significant neutrophilia caused by reactive causes outside the bone marrow. The diagnosis of a LR is based on the exclusion of chronic myelogenous leukemia (CML) and chronic neutrophilic leukemia (CNL). The absence of immature cells, basophilia or monocytosis, and BCR/ABL mutations distinguishes a LR from CML. In CNL, there is marked neutrophilia with no immature cells and, in contrast to a LR, myelocytes, metamyelocytes, and nucleated red cells are infrequent. In our patient, BCR/ABL mutations were negative, and it was felt that having two malignancies at her young age would be the less likely diagnosis.
Common causes of LRs are infection (Clostridium difficile colitis, severe shigellosis, disseminated tuberculosis), malignancy (carcinomas- lung, oropharyngeal, gastrointestinal, genitourinary; melanoma; sarcoma; and Hodgkin’s lymphoma), drugs (steroids, minocycline, G-CSF), ethylene glycol intoxication or severe hemorrhage. The most likely etiologies for this patient include malignancy-associated versus infection. She had no symptoms to suggest C difficile and had no risk factors for tuberculosis. Septic abortion does not commonly cause this extreme a leukocytosis.
Malignancy-associated LRs are commonly observed in lung and kidney carcinomas. Only a number of case reports have described a LR associated with genitourinary tumors. Cervical cancer specifically was mentioned in a 2003 case report in the Annals of Hematology as possibly the first documented. The mechanism of generation of a LR is not well known. It has been postulated that various cytokines produced by the tumor cells, including G-CSF, granulocyte-macrophage colony-stimulating factor (GM-CSF), and IL-6, might explain the pathogenesis.
Overall, this vignette describes an uncommon cause of leukemoid reaction and the pathogenesis. Additionally, it highlights leukemoid reaction as a diagnosis of exclusion and cautions that if overlooked one could miss a hematologic emergency.
2 comments
Jennifer, very interesting case- I would not have thought that this degree of leukocytosis could be due to a LR! I assume the JAK 2 was unrevealing! Great work! Dave
Your case nicely illustrates how the differential is broad for this degree of leukocytosis.