Addressing Barriers to Quitting Cigarettes Among Patients with Opiod Use Disorder
Divya Shankar, MD
RATIONALE:
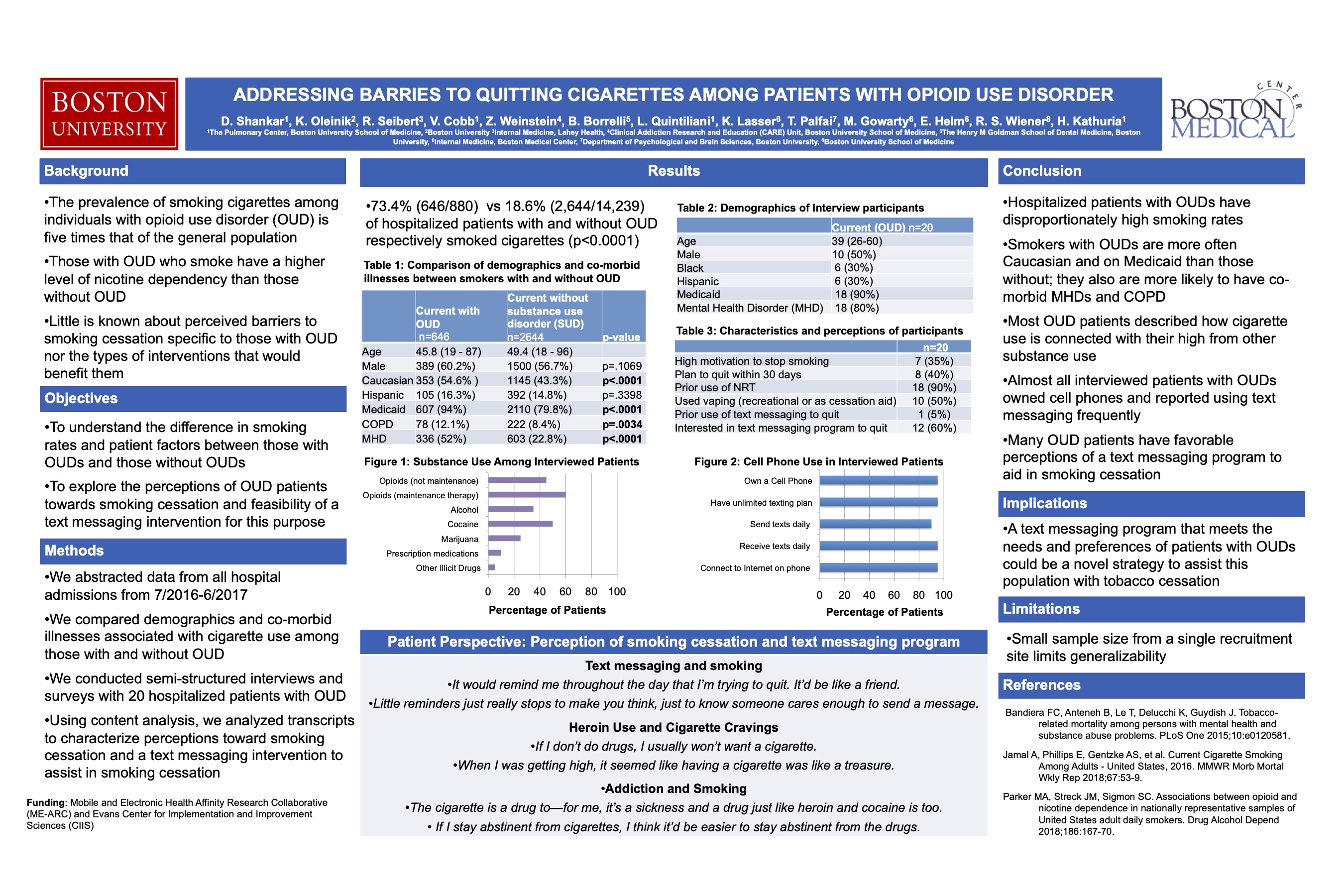
The prevalence of smoking cigarettes among individuals with opioid use disorder (OUD) is five times that of the general population. Not only do those with OUD smoke more heavily, they also have a higher level of nicotine dependency than those without. Hospital-based smoking cessation interventions offer an opportunity to engage with this group of vulnerable patients who may not independently seek treatment for tobacco dependence. Little is known about perceived barriers to smoking cessation specific to those with OUD nor the types of interventions that would match their needs and preferences.
METHODS:
We abstracted data from all hospital admissions between July 1, 2016 and June 30, 2017 and determined demographics, co-morbidities, and cigarette use among those with and without OUD. We then performed a qualitative study entailingsemi-structured interviews with 13 hospitalized smokers with OUD. Using content analysis, we analyzed transcripts to characterize perceived beliefs, attitudes, and barriers to quitting cigarettes among hospitalized smokers with OUD.
RESULTS:
73.4% (646/880) of OUD patients compared to 18.6% (2,644/14,239) of patients without any substance use smoked cigarettes (p<0.0001). Characteristics of patients with OUD were 60.2% (389/646) male, 32.8% (212/646) black, and 16.3% (105/646) Hispanic. The median age was 45.8 (19-87) years. 94% (607/646) were Medicaid insured. There were significant differences in rates of COPD [12.1% (78/646) vs 8.4% (222/2,644), p=0.0034], asthma [16.3% (105/646) vs 9.49% (251/2,644), p<0.0001], and mental health disorders [52.0% (336/646) vs 22.8% (603/2,644), p<0.0001] in smokers with and without OUD respectively. Qualitative analyses showed that many OUD patients believed it was important to quit, especially if they had experienced smoking-related health events. Mistrust of pharmacotherapy, especially varenicline, was a barrier to quitting commonly expressed by patients. Almost all patients described using cigarettes after heroin to enhance the opioid effect. Most patients were interested in using mobile technology to help them quit smoking, and 77% (10/13) of patients reported owning smart-phones.
CONCLUSIONS:
Hospitalized smokers with OUD have disproportionately high smoking rates and co-morbidities and perceive multiple barriers to quitting cigarettes. We found that almost all patients reported how cigarette use potentiates the heroin high, making it critical to de-normalize this behavior to help patients quit both substances. A majority of patients responded positively to the idea of mobile technology to promote smoking cessation. We propose to develop an automated, interactive text-messaging program that addresses mistrust of pharmacotherapy and incorporates OUD patients’ needs and preferences to overcome barriers to quitting cigarettes.
4 comments
HI Divya, Nice work on this project. From my clinical practice caring for patients with a hx of OUD and tobacco use disorder, my patients often tell me that quitting smoking is harder than quitting heroin. Creating a new program to assist this group of patients may make the difference to help them achieve this next goal.
Neat study, Divya. The qualitative data is really helpful in thinking through feasible interventions, and it’s interesting to see the patient perspective on smoking as well.
Divya, terrific work!! The use of mobile apps to help pts with OUD quit smoking is a great example of meeting patients where they are! Well done! Dave
Important and challenging problem. Thanks for tackling it. Given the high rate of mental health disorder, I wonder if substance dependency is a symptom of the underlying disorder and may require more than motivation. David