A Case of Scrofuloderma from Mycobacterium bovis
Ryan Knodle, MD
Learning Objective 1: Diagnose scrofula in patients with painful cervical lymphadenopathy and risk factors.
Learning Objective 2: Recognize and manage the paradoxical upgrading reaction in TB lymphadenitis.
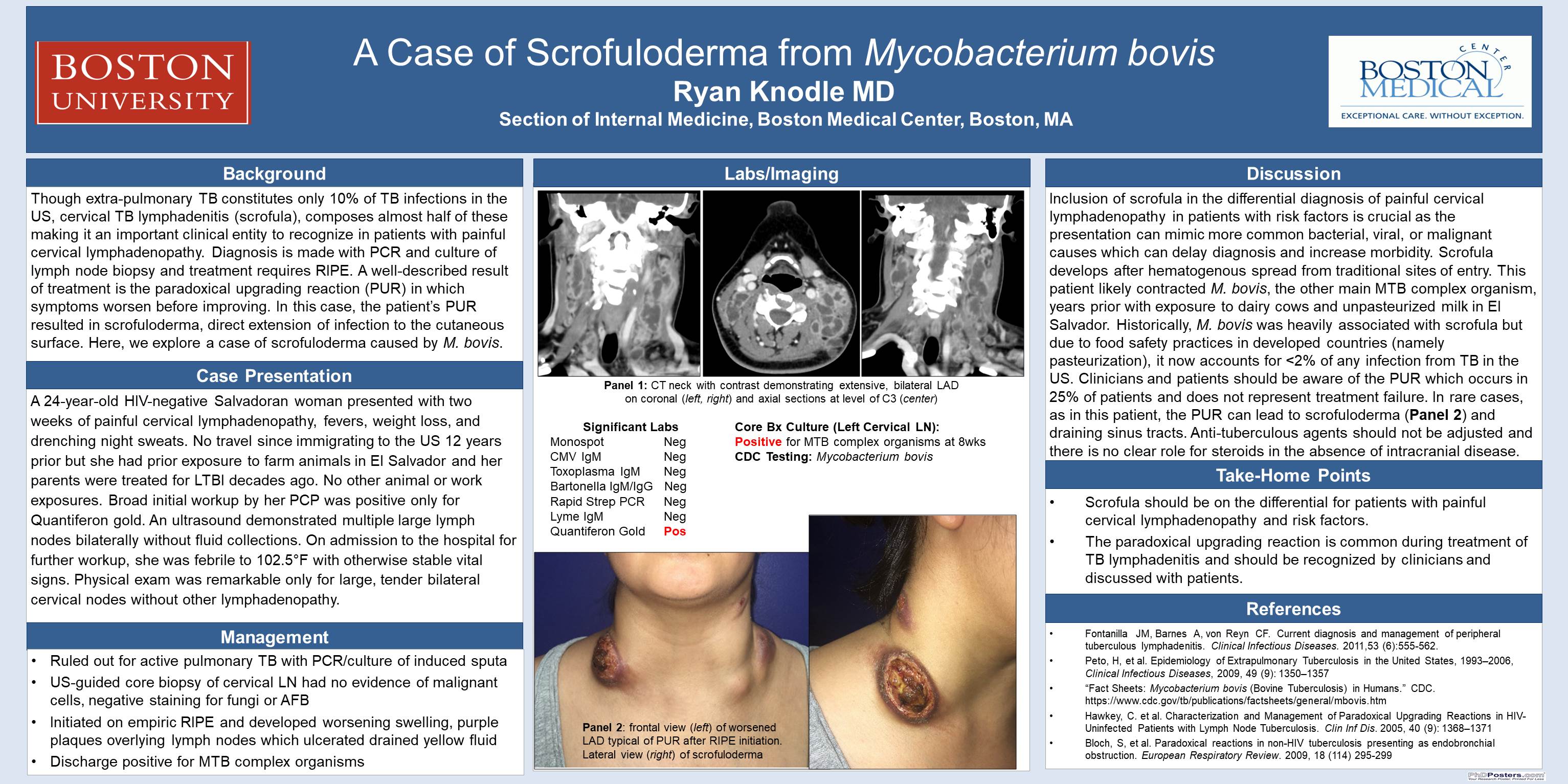
Case: A 24-year-old HIV-negative Salvadoran woman with history of asthma presented with two weeks of painful cervical lymphadenopathy, fevers, weight loss, and drenching night sweats. Though she had not traveled outside of the country since immigrating to the US 12 years prior, she had prior exposure to farm animals in El Salvador and both of her parents were treated for latent TB decades ago. She was employed at a restaurant and had no occupational or other animal exposures. She had initially been evaluated by her PCP who performed a broad work up with normal serum chemistries and complete blood count and included testing for mononucleosis, streptococcal pharyngitis, toxoplasmosis, cat-scratch disease, and Lyme disease, all of which were negative. A superficial ultrasound demonstrated multiple large lymph nodes bilaterally without any fluid collections. An interferon gamma release assay was positive. She was admitted to the hospital for further workup where she was found to be febrile to 102.5°F with otherwise stable vital signs. Physical exam was remarkable only for large, tender bilateral cervical nodes without other lymphadenopathy. Her chest imaging was unremarkable and was ruled out for active pulmonary tuberculosis via PCR and culture of induced sputa. She underwent ultrasound-guided core biopsy of her cervical lymph node which demonstrated necrotic tissue but no evidence of malignant cells and with negative staining for fungi or acid fast bacilli. Cultures were sent and she was started on rifampin, isoniazid, pyrazinamide, and ethambutol empirically for TB lymphadenitis. After initiating therapy, she developed increased swelling in her neck and purple plaques overlying the lymph nodes which subsequently ulcerated and began draining yellow fluid which was positive for MTB complex organisms on PCR testing and AFB smear. Two months later, the original lymph node cultures became positive for MTB complex later identified as Mycobacterium bovis, confirming the diagnosis of TB lymphadenitis with scrofuloderma.
Discussion: While TB lymphadenitis, also known as scrofula, constitutes approximately 10% of extrapulmonary TB, it remains a relatively uncommon presentation of MTB complex organisms in the immunocompetent host. Inclusion of scrofula in the differential diagnosis of painful cervical lymphadenopathy in patients with risk factors is crucial as the presentation can mimic more common bacterial, viral, or malignant causes which can delay diagnosis and increase morbidity. Historically, M. bovis was heavily associated with scrofula but due to food safety practices in developed countries (namely pasteurization), it now accounts for <2% of any infection from TB in the US. Consideration of M. bovis is clinically significant as there is near universal resistance to pyrazinamide. Similarly, paradoxical upgrading reaction (PUR) occurs in up to 25% of patients with TB lymphadenitis and consists of an interval worsening of lymphadenopathy, usually 3-4 weeks after initiation of treatment and can be mistaken for medication non-adherence, pathogen resistance, or new disease process. PUR resolves without specific intervention and steroids are only indicated in the case of intracranial tuberculomas. In this case, that patient’s PUR resulted in scrofuloderma which is a direct extension of deeper infection to the cutaneous surface.
6 comments
Super interesting case. Superb discussion. Thanks Ryan!
Pretty amazing case.
Interesting case! And this case is very educational and you did a good job distilling it to key take-home points.
Ryan, fascinating case and excellent discussion!! Dave
Ryan, what a great presentation! Thanks!
very nice discussion!