Clinical Experience
Equipment
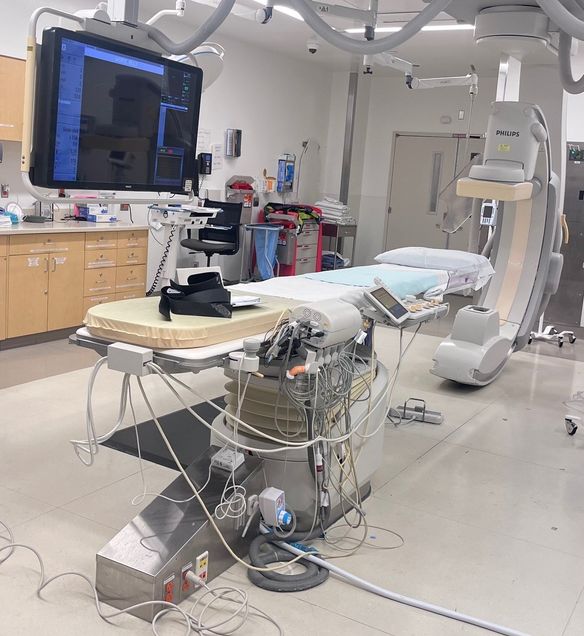
Within the section of Interventional Radiology at BMC, there are 4 fully equipped modern interventional procedural suites for fluoroscopically guided interventions including 1 biplane neuro angiography suite that are each equipped with digital subtraction angiography capabilities. All these suites also include cone-beam CT, post-processing 3-D, image-overlay and roadmap imaging capabilities. There is one CT suite for CT-guided interventions such as thermal ablations, biopsies, drainages, etc. There is a dedicated procedure room for ultrasound guided interventions. Additionally, a minor procedure room is available for venous access and other minor procedures. Anesthesia-supervised sedation can be provided within any of the interventional radiology procedural suites.
Modern diagnostic imaging equipment is present throughout the institution for the performance of medical imaging including 4 modern spectral CT scanners, 3 MRI units, 10 ultrasound units, 1 PET-CT, 1 SPECT-CT, and numerous computed radiography (CR) and digital radiography (DR) units. Duplex vascular imaging is offered in the radiology department and in a dedicated vascular lab.
Similar up to date equipment is present at the VA West Roxbury campus and Children’s Hospital.
Curriculum
The first 3 years of the clinical curriculum are focused on diagnostic radiology (DR) and are identical to the curriculum for those residents in the diagnostic radiology program. The last 2 years are focused on interventional radiology including interventional radiology related and ICU rotations.
The IR clinical curriculum consists of rotations on interventional radiology at BMC and several interventional radiology related rotations. By the conclusion of the residency, IR/DR residents will complete a total of 18 months on interventional radiology, 5 months interventional radiology related rotations and 1 month of ICU. Please refer to the block diagram for more details on the rotations.
Interventional Radiology related rotations:
Intensive Care Unit (ICU) one 4-week rotation during PGY-5 (outside of Radiology)
Vascular Surgery two 4-week rotations during PGY5 and PGY6 (outside of Radiology)
Neurointerventional Radiology two 4-week rotations during PGY5 and PGY6(within radiology)
Musculoskeletal Radiology Procedures one 4-week rotation during PGY5 or 6 (within radiology)

Interventional Radiology Clinic
All faculty members have dedicated time in the interventional radiology outpatient clinic which is held in the surgery specialty clinic space. This is a modern, dedicated clinic space supported by medical assistants and advanced practice providers. Interventional radiology maintains a robust outpatient clinic where consultations are seen and post procedure longitudinal follow up takes place.
During PGY- 5 and PGY- 6, residents will have assigned weekly clinical rotations. The rotation is designed so that the trainee will participate in the dedicated interventional radiology outpatient clinic under the supervision of an attending physician. The resident will perform supervised history and physical examinations on clinic patients and in consultation with faculty will formulate a management plan for each patient, recording all data in the electronic medical record.
While most interventional radiology elective cases are performed on an outpatient basis with same day discharge, those patients requiring admission will be cared by the interventional radiology team. Residents involved in these procedures will handle the admission, procedure related inpatient care, discharge planning and procedure related follow-up.
Additionally, residents will provide ongoing follow-up of hospitalized inpatients who undergo procedures by interventional radiology such as patients undergoing percutaneous drainage, embolization, thrombolysis or other intervention. Residents are responsible for inpatient follow-up and arranging outpatient follow-up in the interventional radiology clinic. Frequently, the resident will personally see the patient he or she was involved in in the inpatient setting at the scheduled outpatient visit to provide for continuity of care.
Responsibilities in these clinical experiences are designed to be progressively expanded over the course of trainee matriculation. For example, a junior level trainee may only have hospital inpatient follow-up responsibilities; whereas, a PGY-5 and PGY-6 resident will provide both inpatient follow-up and outpatient longitudinal care. The overarching goal is to ensure that the supervised resident increasingly assumes the role of the primary clinician in the management of interventional radiology outpatients and inpatients.

Call
IR/DR residents take diagnostic radiology call during their first 3 years similar to their diagnostic radiology resident colleagues. BMC has implemented a night float system for after hours resident diagnostic radiology call coverage. Residents are supervised by attending staff in house overnight. When residents rotate on IR, residents take interventional radiology call from home shared with the other residents on the IR service on a one in every 3 to 4 night frequency. Residents rotating on off-service rotations such as ICU and vascular surgery will take call on those services similar to other ICU or surgical residents. Some of the most interesting and impactful patient experiences take place after hours in both diagnostic and interventional radiology. BMC residents on call are on the front lines of patient care without an additional tier of fellows or advanced trainees to dilute the resident experience.
