Cervical Cancer Screening Rates by Resident & Preceptor Gender
Rebecca Green, MD & Sarah Fulco, MD
TITLE: Gender variations in guideline-concordant cervical cancer screening in resident-preceptor dyads
AUTHORS: Payel J. Roy , Shwetha S. Sequeira , Juhee McDougal , Christine Prifti , Rebecca Green , Sarah Fulco , Mara Eyllon
ABSTRACT BODY:
Background: Prior research has shown that male healthcare providers complete guideline-based cervical cancer screening at lower rates than female providers after completing post-graduate training. This study compared the rates of guideline-concordant cervical cancer screening performed by male and female internal medicine residents among eligible patients in an outpatient general medicine clinic. We then examined whether attending preceptor gender moderated cervical cancer screening completion in these encounters.
Methods: This study was a retrospective chart review conducted on patients seen during an 18-month period at an academic, internal medicine primary care clinic at a safety-net hospital in Boston, Massachusetts. The participants were cisgender female patients between the ages of 24 and 65 who had completed a primary care clinic encounter with an internal medicine resident physician between July 1, 2017 and December 31, 2018. We excluded patients who did not have a cervix. The exposure of interest was male resident gender and the comparator was female resident gender. The outcome of interest was odds of receiving guideline-concordant cervical cancer screening. Data were analyzed using multivariable logistic regression, where we adjusted for patient smoking status, insurance status, and race/ethnicity. In order to understand whether screening varied across preceptor gender, the analyses were stratified by preceptor gender.
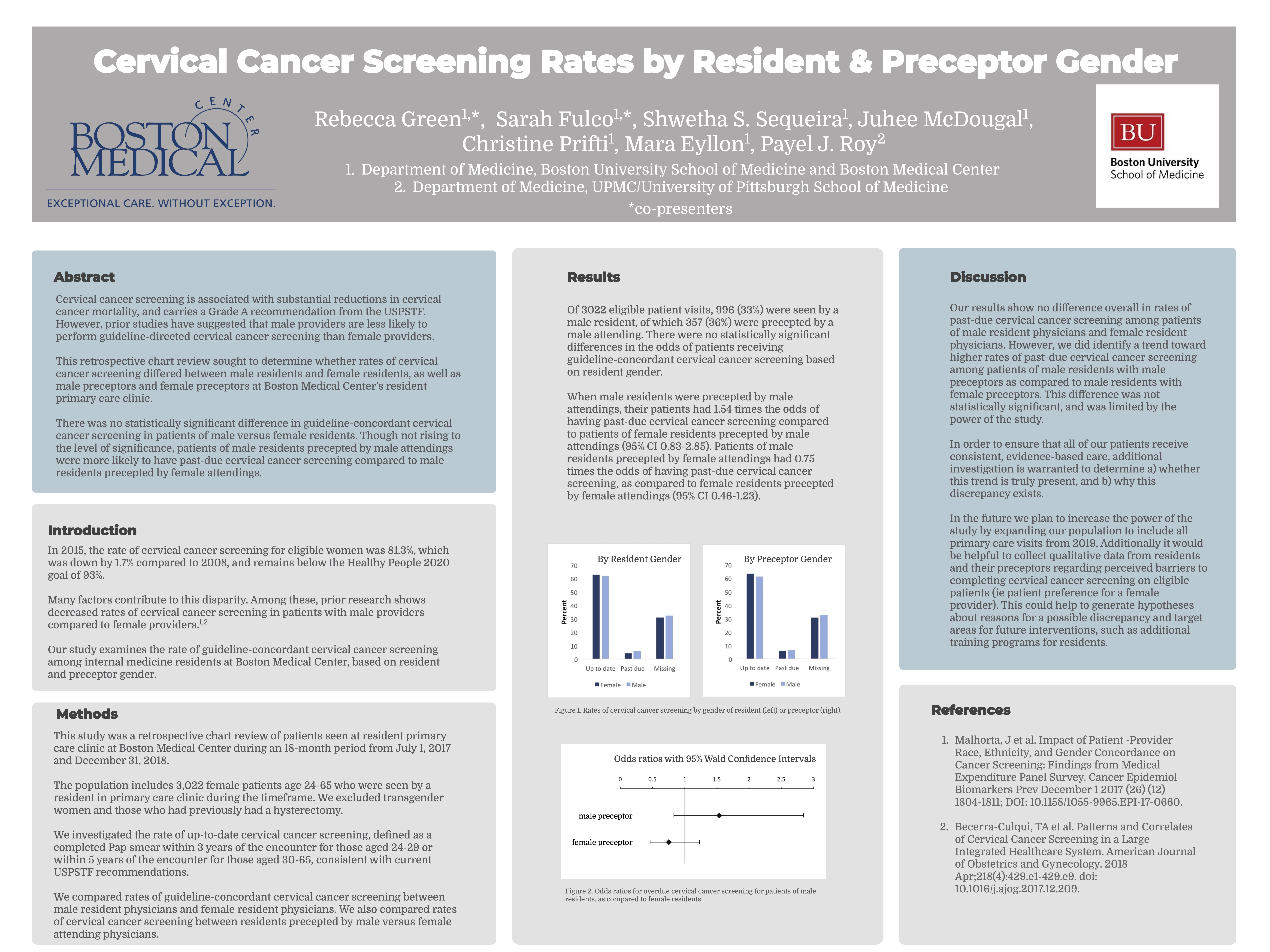
Results: A total of 3,022 patients were included for analysis; 996 were seen by a male resident (33%), of which 357 (36%) were precepted by a male physician. There were no statistically significant differences in the odds of receiving guideline-concordant cervical cancer screening by resident gender. Patients seen by male residents who were precepted by male physicians had 1.54 times the odds of having past-due cervical cancer screening (95% CI 0.83-2.85). When precepted by female physicians, patients of male residents had 0.75 times the odds of past-due cervical cancer screening (95% CI 0.46-1.23). These findings were not statistically significant.
Conclusions: We identified lower odds for cervical cancer screening among cisgender female patients who were seen by male residents with male preceptors compared to male residents with female preceptors. However, the difference was not statistically significant. Our study was limited by statistical power. The identified trend may have implications for the health of female patients cared for by male residents and preceptors. Future directions include increasing the sample size to improve the study’s power and conducting qualitative studies to understand potential reasons for this discrepancy.
5 comments
Rebecca, this is an important study! I hope additional sample size can be obtained since it seems likely that the trends will reach statistical significance with a larger n. Very nicely done!
Dave
this topic is so important, nicely done. It is also complicated to sort out the resident vs. preceptor role and you started to tease that apart. Also, the implications are critical for care delivery if this holds up in a larger study. Nice work.
Great work Rebecca and Sarah. I agree with Dr. Coleman that trend is there and higher sample size might be needed.
Very impressive study. Any chance of extending this to multiple training programs to deal with the sample size and generalizability?
intriguing line of research! I wonder if prior research has investigated gender variations in other non-gyn guidelines as a comparison.