The BEST Center of Excellence
The BEST Center of Excellence aims to improve outcomes for individuals with behavioral health challenges who are vulnerable or underserved, including individuals involved in the criminal justice system, those who are unhoused or unstably housed, or those who repeatedly come into contact with emergency systems as a results of behavioral health challenges. The Center will bring together clinical programs (inclusive of Boston’s Community Behavioral Health Center), training, research and evaluation including to collaborate with community partners and expert colleagues to link datasets and improve understanding of the vulnerable populations served by BEST.
Meet The Team:
Rachel Oblath, Ph.D.
Director of Research Methodology- BMC Department of Psychiatry
Assistant Professor
Boston University Chobanian and Avedisian School of Medicine
 Tasha Ferguson, LMHC
Tasha Ferguson, LMHC
Executive Director, BEST Center of Excellence
Senior Director, Behavioral Health Crisis Continuum
As Executive Director Tasha is responsible for implementing the mission of the BEST Center of Excellence by bringing together a group of clinicians, researchers, educators and community leaders invested in improving outcomes for vulnerable individuals encountering the crisis system of care. Over the past 15 years she has been at the forefront of expanding BMC’s continuum of emergency mental health care, leading the Boston Emergency Services Team (BEST) where she has overseen programs in mobile crisis intervention, community crisis stabilization, behavioral health urgent care, and criminal justice diversion. Under Tasha’s stewardship BEST’s comprehensive model has collaborated with key stakeholders from city and state agencies, law enforcement, community behavioral health providers, area hospitals and more to provide equitable and dignified care for people experiencing behavioral health crisis. She is also a Clinical Instructor at Boston University School of Medicine’s Mental Health Counseling and Behavioral Medicine Program.
 Hayden Lainhart
Hayden Lainhart
Program Coordinator
Hayden works alongside the BEST leadership team to provide project management and data analysis support for the newly established BEST Center of Excellence. Hayden brings a strong background in administrative support, data analytics, and clinical operations including previous experience supporting leadership with data-driven insights and operational planning.
Current Partnership Services:
For the Greater Boston community, BEST currently partners with the City of Boston, Boston Police Department (BPD), the Boston Municipal Courts, the Trial Court of Massachusetts and the Department of Mental Health to provide criminal justice diversion programs designed to provide evaluation and treatment services to individuals with behavioral health problems with the goals of diverting arrests, minimizing incarceration and fostering recovery. These programs include a Police Co-responder Program, Mental Health Court Program and Outpatient Assisted Treatment Program. Through additional support in FY’21 from the City of Boston and federal grants, these programs are being significantly expanded.
The partnership provides a longitudinal collaboration with short and long term goals of changing attitudes, behaviors, and outcomes for citizens of Boston, Boston Police and the criminal justice system through a variety of training and educational opportunities to joint program staff, Boston Police, fellows, community at-large.
BEST Partnership Multicultural Training and Education Initiatives:
- Mental Health and Psychological First Aid for all
- Anti-Racist and Implicit Bias Training- longitudinal engagement
- Case-based Truth and Reconciliation Program- longitudinal learning
- Crisis intervention training
- De-escalation training
- Fellowship in Behavioral Health, Racial and Social Justice
BEST Partnership Data Coordinating Center:
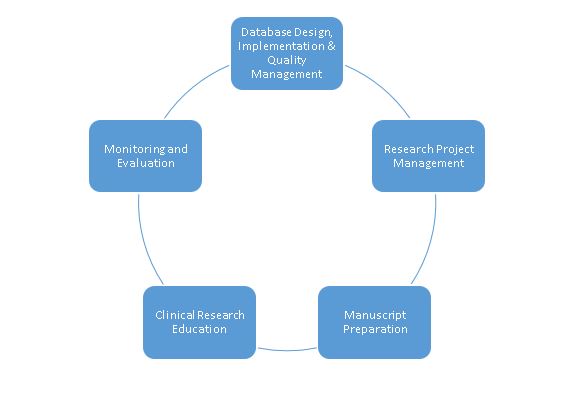
The BEST Partnership for Behavioral Health, Racial, and Social Justice Data Coordinating Center (DCC) offers the necessary resources to house a centralized database linking data from BPD, the Massachusetts Trial Courts, BEST, and the Boston Outpatient Assisted Treatment (BOAT) Program. Our team is comprised of Research Faculty, a research manager and coordinator, data analysts, and research and clinical postdoctoral fellows. Working with program leaders, the DCC team assists in the integration of program services and strengthens partnerships.
Measurable Outcomes:
- Reduction in police arrests
- Reduction in ED visits
- Reduction in duration of psychiatric hospitalizations
- Change in police attitudes
- Implicit Bias trainings for police, court, and behavioral health workforce
- Decrease in unemployment rates among those with mental health disorders
- Improve timely access to high quality behavioral health services
Current Research Projects:
Drs. Rachel Oblath and Kaila Rudolph are currently working on a qualitative analysis of clinical notes for elderly individuals (ages 60 and up) who are experiencing homelessness and use BEST services.
Dr. Rachel Oblath and Elizabeth Plange, in collaboration with Boston EMS, are working on an evaluation of the Alternative Response Model, in which BEST clinicians co-respond to emergencies in the community with EMTs. They are merging data from both BEST and EMS and analyzing important outcomes, including diversion from the emergency department and transport to lower acuity mental health settings.
Publications:
Vrjklan, K., Oblath, R., Black-Ingersoll, F., Grady, S., Burrows, K., Fabian, M.P., Parker, S.E., & Nori-Sarma, A (in press). A case-crossover study of extreme heat and psychiatric emergency encounters among vulnerable pregnant people. Paediatric and Perinatal Epidemiology.
Beaugard, C., Khan, S., Sadatis, C., Oblath, R., & Yule, A (in press). Co-occurring substance use and psychiatric disorders in psychiatric emergency services: Suicidality, substance use, and treatment utilization. Journal of Dual Diagnosis.
Rudolph, K.A., Beaugard, C., Xu, C., Syed, S., Duncan, A., Brown, H.E., Henderson, D.C., & Oblath, R. (2025). Psychiatric emergency service usage trends: Adults experiencing homelessness in Massachusetts from 2005-2020. Journal of Health Care for the Poor and Underserved, 36(1), 240-256. https://doi.org/10.1353/hpu.2025.a951595
Oblath, R., Oh, A., Herrera, C.N., Duncan, A., & Zhen-Duan, J. (2023). Psychiatric Emergencies among Urban Youth during COVID-19: Volume and Acuity in a Multi-Channel Program for the Publicly Insured. Journal of Psychiatric Research, 160, 71-77
Herrera, C. N., Oblath, R., & Duncan, A. (2023). Psychiatric Boarding Patterns Among Publicly Insured Youths Evaluated by Mobile Crisis Teams Before and During the COVID-19 Pandemic. JAMA Network Open, 6(7), e2321798-e2321798
Oblath, R., Herrera, C.N., Were, L.P.O. et al. Long-Term Trends in Psychiatric Emergency Services Delivered by the Boston Emergency Services Team. Community Ment Health J (2022). https://doi.org/10.1007/s10597-022-01015-8
Duncan, A., Herrera, C. N., Okobi, M., Nandi, S., & Oblath, R. (2022). Locked down or locked out? Trends in psychiatric emergency services utilization during the COVID-19 pandemic. Journal of Health Services Research & Policy, 28(2), 80-88
Conference Presentations and Posters:
Fisher, Courtney; Morabito, M.S., Savage, J., and Oblath, R. (2025, April). Identifying points of intervention: A collaboration between the Boston Emergency Services Team and the Boston Police Department. In Tsay, S., Doing Public Administration Differently. Paper presented at the Boston Area Research Initiative Conference, Boston, MA.
Ingersoll-Black, F., Willis, M.D., Grady, S.T., Vrkljan, K., Duncan, A., Burrows, K., Oblath, R., & Nori-Sarma, A. (2025, April). Climate resilience adaptations & psychiatric emergency services use during extreme heat in Boston, MA: a difference-in-differences study. Poster presented at the Boston Area Research Initiative Conference, Boston, MA.
Katkhuda, F., Khan, S., Oblath, R., Vyas, N., Tran, A., Crouse, N., & Trede, K. (2025, April). Community crisis stabilization: Multidisciplinary approach to improving patient care. Poster to be presented at the Together for Hope Conference, Worcester, MA.
Xu, C., & Oblath, R. (2024, October). Racial and ethnic differences in primary mental health outcomes of co-response encounters. Poster presented at the American Public Health Association Annual Meeting, Minneapolis, MN.
Brown, E., Oh, S., Duncan, A., & Oblath, R. (2024, October). Pathways to mental health Care for suicidal Black youth. Poster presented at the American Academy of Child and Adolescent Psychiatry Annual Meeting, Seattle, WA.
Black-Ingersoll, F., Grady, S., Oblath, R., Teigen, K., Herrera, C.N., Fabian, P., Burrows., K., & Nori-Sarma, A. (2024, August). Ambient temperature and psychiatric emergency department visits among unhoused, uninsured, and publicly insured persons. Paper presented at the Annual Meeting of the International Society of Exposure Science, Santiago, Chile.
Syed, S., Herrera, C.N., Oh., S., & Oblath, R. (2024, April). Trends in Psychiatric Emergency Service Use by Asian American Youth Before and During the COVID-19 Pandemic. Poster presented at the Annual Conference of the Society of Pediatric Psychology, New Orleans, LA. **Student Poster Award Winner**
Velez, G., Virani, N., Chava, A., Perez, D.C., Oblath, R., Camacho, L., Roque, K., & Wenzel, S. (2023, May) Influence of implicit racial biases on mental health outcomes reported by the Boston Emergency Services Team (BEST). Poster to be presented at the Annual Meeting of the American Psychiatric Association, San Francisco.
Oblath, R., Herrera C.N., Xu, C., Syed, S., Henderson, D.C., & Duncan, A. (2023, May). Racial and Ethnic Differences in Pathways to Care, Diagnosis, and Disposition among Youth at a Multi-Modality Psychiatric Emergency Services Program. Poster presented at the Annual Meeting of the American Psychiatric Association, San Francisco, CA.
Oblath, R., Xu, C., Herrera, C.N., Henderson, D.C., & Duncan, A. (2023, May). Differences or disparities: Racial patterns in public psychiatric emergency services. In Clarke, D. (chair) When a Difference Becomes a Disparity: Addressing Racialized Inequities in Psychiatric Emergency Treatment. Paper presented at the Annual Meeting of the American Psychiatric Association, San Francisco, CA.
Black-Ingersoll, F., Burrows, K., Grady, S., Teigen, K., Oblath, R., Nori-Sarma, A. (2023, August). Assessing impacts of highly-spatially resolved environmental exposures using electronic health records of understudied populations. Paper presented at the Annual Meeting of the International Society of Exposure Science, Chicago, IL.
Oblath, R., Xu, C., Herrera, C.N., Henderson D.C., & Duncan, A. (2023, November). The school to psychiatric emergency services pipeline: Racial and ethnic differences. In TBD (moderator) Challenges and Solutions to Stigma and Discrimination Experienced by Vulnerable Youth. Paper to be presented at the Annual Meeting of the American Public Health Association, Atlanta, GA.
Khan, S., Beaugard, C.A., Carlin, C., Katkhuda, F., Oblath, R. (2023, December). Substance use and disposition plans for adults with psychosis utilizing psychiatric emergency services. Poster to be presented at the American Academy of Addiction Psychiatry, San Diego, CA.
Other Publications:
Oblath, R., Xu, C., & Plange, E. (2024). Growth through Recovery from Addiction: Participant Experiences in Dorchester Recovery Court. Report for Dorchester Recovery Court Program staff, Boston MA: Boston University Chobanian & Avedisian School of Medicine and Boston Medical Center
Oblath, R., Ferguson, T., Herrera, C.N., & Borba, C.P. (2021). Preliminary Report: Boston Emergency Services Team (BEST) Mobile Team Encounters, 2018-2020. Report for the Mayor’s Office, Boston MA: Boston Medical Center.
Herrera CN. Becoming a candidate for mental health care: a mixed methods investigation of how the process of seeking care contributes to persistent mental health disparities experienced by youth of color. Doctoral Thesis. Published online 2023.
Media:
Youth with public insurance likely to be boarded during COVID”. Herrera C interviewed by Valerie A. Canady, Mental Health Weekly, July 31, 2023. Accessed at https://onlinelibrary.wiley.com/doi/abs/10.1002/mhw.33733
“US had ‘psychiatric boarding crisis’ during COVID-19 pandemic.” Weldon R. Healio. July 7 2023. Accessed at https://www.healio.com/news/pediatrics/20230707/us-had-psychiatric-boarding-crisis-during-covid19-pandemic





