DoM Nurse Receives Nurses Week Provider Partner of the Year Award
Congratulations to DoM's Dr. Christopher Huang for winning one of this year's Nurses Week Provider Partner of the Year Awards, given to providers who are great partners to us in caring for our patients here at BMC! Quotes from nomination letters are below.
"Dr. Huang is the first to recognize exceptional teamwork and its affect on both patient care and patient experience. He frequently sends out full staff emails thanking them for the unit's work that day and encouraging all nurses to connect with him if they have ideas, suggestions, or concerns over anything.
Dr. Huang is inspiring in his perpetual friendly, constant, and can-do outlook on even the most pressing projects. He constantly contributes to collaborative problem solving for all elements of his practice. He is quick to volunteer to call a patient, nurse, or anesthesia provider to make the day run as smoothly as possible.
Dr. Huang has worked tirelessly, via a strong collaboration with administration and nursing leadership, to increase patient access to colorectal cancer screenings. He has continuously interfaced with clinic staff, his fellow endoscopists, and the GI charge nurses to make available the maximum amount of GI screenings possible to make progress on the backlog present since COVID closed many similar units. Dr. Huang utilizes his excellent communication skills to add patients, shuffle attending schedules, and give patients an excellent BMC experience."
DOM Faculty Receives DEIA Recognition Awards
Assistant Professor of Medicine Ricardo Cruz, MD, MPH, MA is one of two to receive the Diversity, Equity, Inclusion & Accessibility (DEIA) of the Year Award. The award recognizes those who have done an extraordinary job at addressing and improving diversity and fostering a culture of inclusion, equity and accessibility throughout the school community.
Cruz joined the faculty in 2014. His clinical work at Boston Medical Center (BMC) focuses on primary care and treatment of substance use disorders and viral hepatitis for vulnerable populations including racial and ethnic minority communities and individuals with history of criminal justice involvement. He also is a physician in the Faster Paths to Treatment, BMC’s innovative, low-barrier, substance use disorder bridge clinic.
His research interests include clinical innovations to address health and treatment disparities among people with substance use disorder. He was the principal investigator of the U.S. Department of Health and Human Services Office of Minority Health-funded Project RECOVER (Referral, Engagement, Coaching, Overdose preVention Education in Recovery), a project that utilizes peer recovery coaches to assist with engagement and retention of individuals with opioid use disorder into treatment and primary care services after completion of acute treatment services (detoxification). He has been a co-investigator on National Institute on Alcohol Abuse and Alcoholism and National Institute on Drug Abuse-funded randomized clinical trials testing medications for alcohol and cocaine use disorders.
Additionally, Cruz serves in the school’s Academy of Medical Educators where he teaches medical students during the preclinical doctoring courses with a focus on development of communication, physical exam, and clinical reasoning skills.
According to another colleague, Cruz educates medical students and residents on the health impact and inequities driven by the criminal justice system. “Dr. Cruz is known as an excellent clinical teacher and his educational scholarship is deeply tied to the values of antiracism.”
DOM Faculty Appointments and Promotions – March 2024
Professor
Stefano Monti, PhD, Medicine/Computational Biomedicine, integrates systems biology, machine learning and bioinformatics approaches to investigate the molecular drivers of human disease, with the goals of advancing prevention and care. This multidisciplinary effort relies on the development of novel computational methodologies, and on the design of experiments based on the generation and integrative analysis of high-throughput multi-omics data, with the goal of identifying novel therapeutic targets and developing accurate diagnostic and prognostic biomarkers. Dr. Monti’s areas of research include the study of the molecular mechanisms of tumor initiation and progression and of the role played in it by environmental exposure, with funded projects in head and neck cancer and breast cancer, as well as the study of the biological factors contributing to healthy aging and extreme longevity. His lab also led the computational studies of genomic events associated with diffuse large B cell lymphoma that could provide prognostic biomarkers for that disease.
DoM Education Week – May 20-24
The Department of Medicine will hold its first Education Week from May 20th through May 24th. There will be a series of activities for educators, administrators, and trainees with the hope to promote a sense of community, foster collaborations in teaching, and celebrate educational success at DOM. Please check out the agendas below for more details and RSVP HERE if you are interested in participating in any of the sessions. We look forward to seeing you there!
DoM Faculty Receives Million Research Partnership to Intercept Lung Cancer From American Lung Association and the LUNGevity Foundation
WASHINGTON, DC (April 9, 2024) – Lung cancer remains the leading cause of cancer deaths in the United States, with someone diagnosed approximately every two minutes. In a collaborative effort to end this devastating disease, the American Lung Association and LUNGevity Foundation have joined forces to invest $3 million over the next three years in research aimed at intercepting lung cancer – catching precancerous cells and blocking them from turning into cancer cells.
This ongoing partnership brings together leading scientists dedicated to investigating early molecular and other changes that lead to cancer development, with the ultimate goal of stopping lung cancer before it begins. By focusing on early detection and intervention, the research aims to significantly improve survival rates and outcomes for patients.
"Early detection of lung cancer is crucial to saving lives. By investing in research to intercept lung cancer at its earliest stages, we have the potential to revolutionize how we approach this disease and improve outcomes for patients,” said Harold Wimmer, president and CEO of the American Lung Association.
"Continuing our partnership with the American Lung Association to help stage-shift lung cancer underscores our commitment to advancing research that will make a tangible difference in the lives of those affected by the disease. Together, we are harnessing the power of scientific innovation to drive progress in interception strategies and potentially cure lung cancer,” said Andrea Ferris, president and CEO of LUNGevity Foundation.
The partnership will fund research co-led by Avrum Spira, MD, MSc, and Steven Dubinett, MD, PhD, under the project titled “Intercept Lung Cancer Through Immune, Imaging & Molecular Evaluation InTIME.” This research aims to establish a timeline of precancerous cell evolution into malignant cancer, utilizing cutting-edge technologies such as robot-assisted bronchoscopy to collect longitudinal samples from patients suspected to have lung cancer. Dr. Spira, Global Head of Interventional Oncology at Johnson & Johnson and Professor of Medicine at Boston University, and Dr. Dubinett, Dean of the David Geffen School of Medicine at UCLA, are leaders in the field of lung cancer research.
"This project represents an evolution of our ongoing efforts to understand and intercept lung cancer before it progresses," said Dr. Spira. "By unraveling the molecular and immune mechanisms underlying lung cancer development, we can develop targeted strategies for early detection and intervention."
The partnership builds upon previous collaborations, including research funded by the American Lung Association, LUNGevity Foundation, and Stand Up To Cancer, which has yielded significant findings in lung cancer interception. Notable achievements include mapping the precancer genome, the discovery of enzymes and proteins associated with premalignant cells, and offering potential targets for treatment, as well as insights into immune cell activity in premalignant lesions. Partial funding was provided by the Thomas G. Labreque Foundation.
Through initiatives like the American Lung Association Research Institute Accelerator Program and the LUNGevity Early Lung Cancer Center, this partnership aims to accelerate progress in lung cancer interception research and pave the way for personalized treatments for patients.
For more information on the American Lung Association and LUNGevity Foundation, visit Lung.org/intercept-cancer and LUNGevity.org.
About LUNGevity Foundation
LUNGevity, the nation’s leading lung cancer organization, is transforming what it means to be diagnosed and live with lung cancer. LUNGevity seeks to make an immediate impact on quality of life and survivorship for everyone touched by the disease—while promoting health equity by addressing disparities throughout the care continuum.
- Through research, we use an innovative and holistic approach to finding lung cancer earlier when it is most treatable; advance research into new treatments so people may live longer and better; and ensure a diverse, vital pipeline of investigators for the future of the lung cancer field.
- Through advocacy, we foster groundbreaking collaborations to ensure all people have access to screening, biomarker testing, and treatment breakthroughs.
- Through community, we educate, support, and connect people affected by lung cancer so that they can get the best healthcare and live longer and better lives.
Comprehensive resources include a medically vetted and patient-centric website, Patient Gateways for specific types of lung cancer, a toll-free HELPLine for personalized support, international survivor conferences, and tools to find a clinical trial. All these programs are designed to help us achieve our vision—a world where no one dies of lung cancer. LUNGevity Foundation is proud to be a four-star Charity Navigator organization.
Please visit www.LUNGevity.org to learn more.
About the American Lung Association
The American Lung Association is the leading organization working to save lives by improving lung health and preventing lung disease through education, advocacy and research. The work of the American Lung Association is focused on four strategic imperatives: to defeat lung cancer; to champion clean air for all; to improve the quality of life for those with lung disease and their families; and to create a tobacco-free future. For more information about the American Lung Association, which has a 4-star rating from Charity Navigator and is a Platinum-Level GuideStar Member, call 1-800-LUNGUSA (1-800-586-4872) or visit Lung.org. To support the work of the American Lung Association, find a local event at Lung.org/events.
About Lung Cancer in the US
- About 1 in 16 Americans will be diagnosed with lung cancer in their lifetime.
- More than 238,000 people in the US will be diagnosed with lung cancer this year.
- About 60%-65% of all new lung cancer diagnoses are among people who have never smoked or are former smokers.
- Lung cancer causes more deaths than the next two deadliest cancers (colorectal and pancreatic) combined.
- Only 25% of all people diagnosed with lung cancer will survive 5 years or more, but if it’s caught before it spreads, the chance of 5-year survival improves dramatically.
Asher Tulsky, MD, Named Distinguished Faculty of the Month for April
The Faculty Affairs Office is pleased to announce that Associate Professor of Medicine Asher Tulsky, MD, has been named April’s Distinguished Faculty of the Month.
He joined our community in December 2015. Currently, he serves as associate chief for education in the Section of General Internal Medicine in the Department of Medicine. He is also director of resident development in the internal medicine residency program at Boston Medical Center where he established and runs the professional development coaching program and directs the remediation program for residents in need. In addition, he has served on numerous school committee, including the Medical Education Committee, Student Evaluations and Promotions Committee, BU Medical Group’s Communications, Faculty Development and Wellness committees.
His nominators said, “These positions reflect his dedication to continuous improvement of the medical education system and student welfare.
“Dr. Tulsky is an outstanding educator with a deep and thoughtful commitment to meeting learners where they are, recognizing their needs and supporting them to achieve their best. He always looks for opportunities to give feedback constructively to encourage personal and professional growth. He focuses on learners facing challenges, looking for ways to engage and encourage them.
“He has provided invaluable guidance and support to numerous students, fostering their academic and professional growth.
Dr. Tulsky is “a tireless advocate for promoting clinician educators.”
Congratulations!
Researchers Awarded $14 Million to Better Understand, Treat Genetic Lung Diseases
A team of researchers led by Darrell N. Kotton, MD, the David C. Seldin Professor of Medicine, has been awarded a five-year, $14 million grant from the NIH’s National Heart, Lung, and Blood Institute (NHLBI) for his research, “Developing Pluripotent Stem Cells to Model and Treat Lung Disease.”
Lung diseases, such as those caused by gene mutations, result in significant morbidity and mortality worldwide. The advent of stem cell discoveries and regenerative medicine presents new opportunities to improve the understanding of these diseases and to develop new treatment approaches.
The new award will fund an integrated, multi-investigator program project grant where four interacting labs headed by four physician-scientists, all located in the Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center, will develop next generation stem cell-based therapies for currently incurable genetic lung diseases affecting children and adults, including childhood and adult interstitial lung diseases, an inherited form of emphysema, cystic fibrosis and primary ciliary dyskinesia.

The four physician-scientists heading each lab include Kotton together with Professor of Medicine, Andrew A. Wilson, MD, Associate Professor of Medicine, Finn Hawkins, MBBCh, and Assistant Professor of Medicine, Kostas Alysandratos, MD, PhD. The four teams have worked closely together for several years on stem cell-based approaches for treating lung disease, including throughout the pandemic when they famously shared their stem cell bank with researchers across the world to develop new models for understanding and treating COVID-19.
“While it is hard to envision a more optimistic time in health-related research, treatments for many devastating lung diseases have not yet been realized, and clinical therapies in many cases still largely focus on treating symptoms,” says Kotton.
For the new project, Kotton and his teams have developed reprogramming methods to generate induced pluripotent stem cells (iPSCs) from patients and have applied these methods to produce the largest known bank of lung disease-specific iPSCs. Having established these stem cell banks and protocols, Kotton now is focused on applying these resources to advance their mechanistic understanding of how gene mutations initiate airway and alveolar epithelial dysfunction resulting in disease. They seek to intervene with precision therapeutics or regenerative cell therapies. According to Kotton, they will focus initially on ameliorating or curing genetic lung diseases of the airway and alveoli, given that their proximal disease-driving gene mutations are well described.
“The researchers on this new project are not new to this mission, for they have worked together for many years in juxtaposed labs, publishing an extensive literature that provides a solid foundation upon which to now launch a concerted effort to move our field from basic discovery to therapeutic development,” said Kotton.
Kotton is an Allen Distinguished Investigator and an elected member of the American Society of Clinical Investigators and Association of American Physicians. He leads a basic research laboratory, continuously funded by the NIH since 2004 and serves on the NHLBI’s Board of External Experts. He is the recipient of the American Thoracic Society’s Recognition Award for Scientific Accomplishments (2018), the AAMC inaugural national Research Resources Sharing Award (2017), the Alpha-1 Foundation’s Researcher of the Year (2013) and Shillelagh (2010) awards, Boston University’s Graduate Medical Sciences Educator of the Year Award (2018), and the Robert Dawes Evans Senior Research Mentor Award from Boston University.
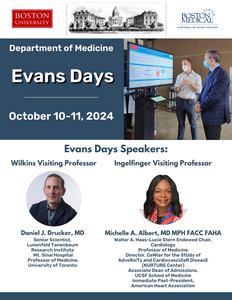
2024 Evans Days Speakers Announced! October 10-11, 2024
Dr. Andrew Wilson Promoted to Professor of Medicine
Join us in congratulating Dr. Andrew Wilson on his promotion to Professor of Medicine in the section of Pulmonary, Allergy, Sleep & Critical Care Medicine. 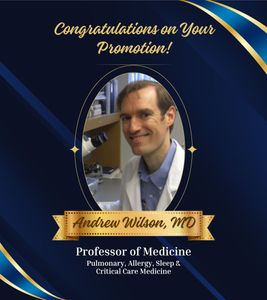
DoM Faculty Member Receives 2024 Sexual Medicine Research Fund Award
Join us in congratulating Jai Marathe, MBBS, MS in receiving the 2024 Sexual Medicine Research Fund Award!
Jai Marathe, MBBS, MS, assistant professor of medicine/infectious diseases, and her team are developing monoclonal antibody-based products that can prevent sexually transmitted infections as well as pregnancy. Complement proteins participate in a number of antibody mediated immunological functions such as cell lysis, opsonization/phagocytosis and chemotaxis. The researchers will measure complement levels and activity in vaginal secretions and study the diffusion and function of a contraceptive anti-sperm antibody (Anti-CD52g) in vaginal and cervical mucus.


