Dr. Kevin Wilson Among Expert U.S. Panel that Developed NIH COVID-19 Treatment Guidelines
 Kevin Wilson, MD, professor of Pulmonary, Allergy, Sleep & Critical Care Medicine, is among a panel of 30 U.S. physicians, statisticians and other experts which has developed treatment guidelines for coronavirus disease 2019 (COVID-19).
Kevin Wilson, MD, professor of Pulmonary, Allergy, Sleep & Critical Care Medicine, is among a panel of 30 U.S. physicians, statisticians and other experts which has developed treatment guidelines for coronavirus disease 2019 (COVID-19).These guidelines, intended for healthcare providers, are based on published and preliminary data and the clinical expertise of the panelists, many of whom are frontline clinicians caring for patients during the rapidly evolving pandemic. The guidelines are posted online (covid19treatmentguidelines.nih.gov) and will be updated often as new data are published in peer-reviewed scientific literature and other authoritative information emerges.
DOM Faculty Insights on COVID-19
Joshua Barocas, MD
KISS 108 Matty in the Morning | Dr. Joshua Barocas Calls In
Huffington Post | Social Distancing: Can You Hang Out With Friends If You Stay 6 Feet Apart?
STAT | The coronavirus pandemic could transform our health care system — for the better
WBUR | Hospitals Seeing Rise In Coronavirus Cases A Week Before Predicted Peak
Newsweek | CORONAVIRUS STAYED IN WOMAN'S EYES FOR 20 DAYS
Tracy Battaglia, MD, MPH
BU Today | Coronavirus Thank-you Notes from the BU Community
Nahid Bhadelia, MD, MA
Mother Jones | Can COVID-19 Be Treated? Does Blood From Survivors Help? Experts Answer Our Questions on Antibodies.
Yahoo Finance | Avoid Twitter’s swamp of misinformation by following these epidemiology experts
MSNBC | Doctor: Many medical centers ‘stopped recommending’ malaria drugs for COVID-19-19
Gizmodo | Report: HHS Put Aide Nicknamed the 'Dog Breeder,' an Actual Dog Breeder, in Charge of Virus Response
Natasha Hochberg, MD, MPH
Women’s Health | What to Know About the Survival Rate of Coronavirus
Yahoo Lifestyle | How are hospitals preparing for the coronavirus peak? Yahoo News Explains
James Hudspeth, MD, FACP
Gerald T. Keusch, MD
Live Science | Wuhan lab says there's no way coronavirus originated there. Here's the science.
Vox | Scientists explain why it’s unlikely the coronavirus escaped from a Chinese lab
WKU | Your Coronavirus Questions, Answered
Benjamin P. Linas, MD
Aditya Mithal, PhD; George J. Murphy, PhD; Richard Giadone, PhD
George J. Murphy, PhD
Nature | Thousands of coronavirus tests are going unused in US labs
The Scientist | Logistical Hurdles Leave COVID-19 Test Kits Unused
Nature | Untapped potential: More US labs could be providing tests for coronavirus
Tuhina Neogi, MD
Medical Dialogues | Long-Term Prescription Opioid Use Associated With Obesity
Raj Parikh, MD
Thomas T. Perls, MD
The Conversation | The CDC now recommends wearing a mask in some cases – a physician explains why and when to wear one
Quartz | Social distancing isn’t the right language for what Covid-19 asks of us
Jeffrey Samet, MD, MA, MPH
USA Today | 'The world is going to hell': Coronavirus can be deadly for people recovering from addiction
Kevin C. Wilson, MD
MDMagazine | American Thoracic Society Releases Temporary COVID-19 Guidance
GIM’s Debra Paarz Awarded BU’s 2020 Perkins Award
BU’s 2020 Perkins Awards for Distinguished Service Announced
Awardees Colin Riley, Kim Richards, Debra Paarz will be honored at a ceremony held later
Congratulations to Debra Paarz
A quarter-century BU veteran, Paarz has spent most of the last two decades with MED’s 120-instructor general internal medicine section, currently serving as its administrator—which now means, among other things, she says, that she’s kept busy supporting leaders, doctors, and nurse practitioners “as their involvement ramps up with COVID-19–related activities.”
In circumstances not involving emergencies like that, she oversees such matters as faculty recruiting, retention, services, promotions, and efforts to counter burnout. She also helps manage clinical and research activities.
“From the moment you join the faculty,” one nominator wrote, “Debbie is there to support you in all aspects, ranging from identifying your mentors, clarifying your clinical schedule, completing your educational expectations, monitoring your clinical performance, maintaining your licensure/certification, applying for intra- and extra-mural funding, and pursuing academic promotion.” Another said that thanks in part to Paarz, the section is reputed “as one of the strongest and most academically productive GIM units nationally.”
From the BU Today story written by Rich Barlow.
Appointments & Promotions – Spring ’20
Congratulations to all faculty recently promoted and welcome to all recent appointments!
Promotions
Fuzhong Qin, Professor
Cardiovascular Medicine
Nahid Bhadelia, Associate Professor
Infectious Disease
Karen Jacobson, Associate Professor
Infectious Disease
Hans Meier Ewert, Clinical Associate Professor
Cardiovascular Medicine
Liu Gang, Research Associate Professor
Computational Biomedicine
Kei Yasuda, Assistant Professor
Nephrology
Appointments
Avik Chatterjee, Assistant Professor
General Internal Medicine
Simeon Kimmel, Assistant Professor
General Internal Medicine
Thomas Ku, Assistant Professor
General Internal Medicine
Charmaine Lastimoso, Assistant Professor
General Internal Medicine
Eric Marks, Assistant Professor
Hematology & Oncology
Stephanie Robinson, Assistant Professor
General Internal Medicine
Hossein Sadrzadeh, Assistant Professor
Hematology & Oncology
Derin Tugal, Assistant Professor
Cardiovascular Medicine
Xiao Yang, Assistant Professor
General Internal Medicine
Archana Asundi, Research Assistant Professor
Infectious Disease
Courtney Faiella, Instructor
Cardiovascular Medicine
Sean Feng, Instructor
Geriatrics
Emily Johnson, Instructor
Cardiovascular Medicine
Vanny (Trieu) McLean, Instructor
Geriatrics
Luke Pak, Instructor
General Internal Medicine
Emily Scarbo, Instructor
Geriatrics
Nebulla Stephen, Instructor
Hematology & Oncology
Intern Match 2020
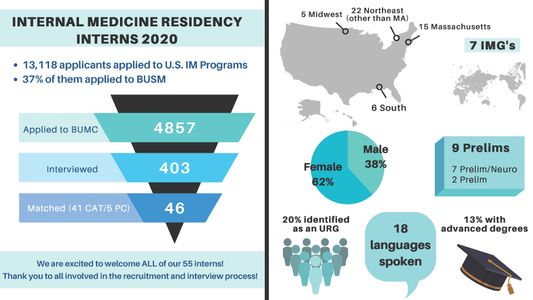
Despite the current clinical challenges posed by COVID-19, medical students and faculty alike recently celebrated the results of the 2020 NRMP Match! Boston Medical Center Internal Medicine Residency program is thrilled to welcome a competitive and diverse class of incoming interns, some of whom will be receiving their Medical Degrees early to join hospital staffs during this epidemic. Congratulations to all of our fourth year medical students and to all of the incoming interns who we will be seeing in June!
With an impressive 37% of all internal medicine applicants applying to BMC, 46 categorical and 9 preliminary interns were matched into the 2020 intern class. As a medical center committed to inclusion and equity, we are proud to welcome interns that are diverse in a number of different measures, from where they graduated medical school to life experiences, interests and passions.
This exceptional group of interns matched to our institution is a reflection of the dedicated group of faculty interviewers that devoted their time to meeting with all 403 candidates. Thank you for demonstrating the mission of this department, the School of Medicine and the hospital and your tireless commitment to our trainees.
Emelia Benjamin, MD Receives AAIM Diversity, Equity and Inclusion Award
 Emelia J. Benjamin, MD, ScM, FACC, FAHA, Vice Chair for Faculty Development and Diversity in the Department of Medicine at BUSM and BMC and BUMC Assistant Provost for Faculty Development, will receive the 2020 Alliance for Academic Internal Medicine (AAIM) Diversity, Equity and Inclusion Award.
Emelia J. Benjamin, MD, ScM, FACC, FAHA, Vice Chair for Faculty Development and Diversity in the Department of Medicine at BUSM and BMC and BUMC Assistant Provost for Faculty Development, will receive the 2020 Alliance for Academic Internal Medicine (AAIM) Diversity, Equity and Inclusion Award.
“Through her world-class research program in cardiovascular epidemiology, remarkable success in program development, and prodigious mentoring activities, she has very positively influenced the careers of faculty from very diverse backgrounds including individuals working to identify and mitigate health disparities,” said Dr. David Coleman, Wade Professor and Chair, Department of Medicine, and Physician-in-Chief at BMC.
Seeking Volunteers for Committee to Establish Principles for Expense Reduction in the DOM
In view of the anticipated substantial reductions in clinical revenue during the COVID 19 pandemic, we are establishing a Committee to Establish Principles for Expense Reduction in the Department of Medicine.
David Coleman, M.D.
Dept COVID-19 Update
Colleagues,
I wanted to update you on a few departmental and institutional activities, and to also express my gratitude for your generous and diligent support of one another and the needs of our patients.
PPE: A number of you have expressed legitimate concern about the restricted availability of PPE, particularly masks, beyond those healthcare workers with direct care responsibilities of COVID 19 confirmed or suspected cases. N95 masks for the ED personnel have recently been made available since they are at high risk. The rationale for making the difficult choice of not distributing masks to everyone include the following: this practice is not currently recommended by CDC and our ID advisors did not believe it was likely to be helpful; since our PPE supply, including masks is limited, conserving available supplies to avoid situations where we don't have sufficient PPE for high risk exposures is a priority. Partners decided to take that chance, we (and other health systems in Boston) did not; I was on a call yesterday with about 25 chairs of medicine-none of their institutions had gone to the full mask policy that Partners implemented. The rationale was the same as ours. The current policy is subject to ongoing revision as the PPE supply becomes clearer. I also wish we had enough masks for everyone but believe that BMC leadership made the correct decision under the circumstances. As to the approach for individuals wearing masks against policy, we decided against requiring staff to remove them despite the unintended message that selective wearing of masks may send. Major efforts are underway to address the PPE supply problem for the institution.
Staffing: Thanks to the hard work of our inpatient COVID teams, led by James Hudspeth, a contingency plan for the anticipated surge in COVID-infected patients is being developed. Our residents and faculty have been remarkably generous in providing coverage, volunteering for service, and supporting one another. The ICU and hospitalist attendings have been particularly effective and supportive in insuring the quality of care and in supervising our hard-working residents! BMC leadership has also been working diligently to expand our potential Med Surg and ICU capacity should the need arise. I anticipate that we will need to extend staffing beyond the usual inpatient medicine and intensive care attending and resident pools if the more extreme surge scenarios occur.
Financial Impact: The financial consequences of the COVID 19 epidemic are obviously being felt across all sectors of the economy, but particularly in the health care industry. The scale of impact across the country is so large that it seems highly likely that there will be some form of government support for the industry. BMC and our department are beginning to experience what is anticipated to be a sharp decline in clinical revenue. In addition, the distribution of clinical work across our department is highly variable-we have some clinicians who are working beyond their usual schedule under very stressful conditions and others who are under-utilized, particularly in the outpatient and procedural areas. It is critically important that we have a thoughtful, responsible, and fair approach to meeting the inevitable financial challenges before us. Therefore, we are forming a committee to develop a set of principles to maximize our ability to support our faculty and staff, and to secure the long-term future of the department. We hope to formulate a plan in the next few weeks. Meanwhile, BMC is seeking permission from the Board of Trustees to implement a furlough plan for BMC employees that seeks to offer some protection for the impacted employees while meeting the financial constraints of the institution.
Communication: The social isolation that we are experiencing is quite daunting. I have been reminded of how meaningful the social interactions are in my own professional life. I do hope to join with you in finding new ways to stay connected. I will hold a departmental faculty meeting via Zoom in the next few days. I encourage each of your sections to continue as many educational activities as possible during this period as well. Please offer any suggestions for how we can improve our communications in the department!
As we endure this unprecedented period of disruption in our personal and professional lives, I am inspired by your kindness and commitment to the noblest values of our profession. Thank you for your forbearance and for working so hard on behalf of our patients and one another. Our department will emerge from this experience wiser, appreciative, and fully prepared to soar into the future!
David Coleman, M.D.
From Cancer Patient to Medical Student
The clinical teams at Boston Medical Center provide interdisciplinary, compassionate care that saves lives.
DOM Experts Weigh-In on COVID-19
Joshua Barocas, MD, Infectious Diseases
WBUR
More Of Your Questions About The Coronavirus, Answered
Tamar Barlam, MD, Infectious Diseases
Boston Globe
Boston’s infectious disease specialists’ message to the public: Don’t be cavalier about the coronavirus
Nahid Bhadelia, MD, MA, Infectious Diseases
ABC News
Best practices to take action against COVID-19
Natasha S. Hochberg, MD, MPH, Infectious Diseases
WBUR
Your Questions About U.S. Travel And The Coronavirus, Answered
Thomas Perls, MD, Geriatrics
The Conversation
Social distancing: What it is and why it’s the best tool we have to fight the coronavirus
