Emelia Benjamin, MD, ScM, Named Jay and Louise Coffman Professor of Vascular Medicine
We are delighted to announce that Emelia J. Benjamin, MD, ScM, will be named the Jay and Louise Coffman Professor of Vascular Medicine effective Oct. 1. A professor of medicine at the Chobanian & Avedisian School of Medicine and professor of epidemiology at BU School of Public Health, Dr. Benjamin has been a Framingham Study investigator since 1988 and a Boston Medical Center attending cardiologist since 1990.
Dr. Benjamin is an international leader in cardiovascular medicine. Her research has been continuously funded by the National Institutes of Health since 1998 for studies of atrial fibrillation, vascular function, inflammation and chronic pain. She has more than 850 publications and an H-index of 215. Her citation ranking internationally is #98 in medicine and #7 for women scientists; nationally her ranking is #71 in medicine and #5 for women scientists.
Dr. Benjamin has held many leadership roles for the American Heart Association since the 1990s and was the recipient of the 2022 American Heart Association Distinguished Scientist Award. She has devoted substantial effort to mentoring, faculty development and coaching of diverse individuals in health sciences and medicine. Her many accolades include the 2020 Alliance for Academic Internal Medicine Diversity and Inclusion Award and the 2024 American Heart Association Louis B. Russell, Jr. Memorial Award for Diversity. Dr. Benjamin is the department of medicine’s inaugural vice chair for faculty development and diversity and the inaugural Medical Campus associate provost for faculty development.
Please join us in celebrating Dr. Benjamin and her achievements as a scholar, mentor, and clinician. Her many contributions to our institution and to the field of cardiovascular medicine make her a deserving recipient of the prestigious Jay and Louise Coffman Professorship of Vascular Medicine.
DoM Bridge Funding Awardees!
The talented awardees all have inspiring and innovative research areas of focus, in key areas that impact our patients’ health and well-being.
Please join us in congratulating the following people:
Dr. Karen Jacobson, Department of Medicine, Section of Infectious Disease. Dr. Jacobson’s expertise is in studying tuberculosis transmission and outcomes. Dr. Jacobson’s research, which spans national and global work, has a particular emphasis on understanding how substance use impacts on tuberculosis transmission and response to therapy.
Dr. Naomi Ko, Department of Medicine, Section of Hematology-Oncology. Dr. Ko’s research has a translational focus directed to understanding the disconnect between scientific discoveries in cancer treatment and delivery of evidence-based treatment to marginalized, racial/ethnic minority women with breast cancer. She is actively investigating how tumor biology, poverty, communication and treatment influence breast cancer outcomes in diverse breast cancer populations.
Dr. Maureen Dubreuil, Department of Medicine, Section of Rheumatology. Dr. Dubreuil’s research focuses on comorbidities and pharmacoepidemiology of spondyloarthritis. (note: Dr. Dubreuil’s bridge funding award is co-funded by BMC and the Department of Medicine)
Dr. Emily Hurstak, Department of Medicine, Section of General Internal Medicine. Dr. Hurstack’s conducts clinical research around improving outpatient systems of care for patients who have been economically and socially marginalized, with a focus on individuals with substance use disorders (SUD) and chronic pain syndromes. Dr. Hurstak participates in both clinical care and research with a focus on health communication, health literacy, and improving care for patients with SUDs in primary care settings.
Dr. Titi Ilori, Department of Medicine, Section of Nephrology. Dr. Ilori’s research includes mechanistic and interventional studies on the etiologic factors and modifiers of chronic kidney disease (CKD), with a special emphasis on the effect of diet (dietary nutrients and dietary patterns), biomarkers, and genetics on CKD progression in both low resource and high-income countries. Her current work is in gene by environment interactions in APOL1 nephropathy and her lab recently discovered that dietary potassium interacts with the APOL1 genotypes.
DoM 2024 Research Publications, New Research Grants & Foundation Awards of Note!
Research Publications: Our faculty continue to receive significant mainstream media coverage for their exceptional published research.
- Kimberly Bertrand’s study in the journal Environmental Research reported long-term use of chemical hair relaxers by postmenopausal Black women was associated with increased risk of uterine cancer.
- Elizabeth Pearce’s study in JAMA Network Open found hyperthyroid patients treated with surgery had a lower risk of death and a lower risk of major adverse cardiovascular events than patients treated with medication.
- Tuhina Neogi’s study in in the journal Arthritis & Rheumatology found calcium crystal deposits in the knee contribute to joint damage.
New Research Grants: Here are our Academic Year 2024’s largest new/renewal grants:
| PI | $ millions | Title (All NIH funded) |
| Rosenberg | 14.5 | Lifetime stressors and Alzheimer's Disease genetic variants and biomarkers in relation to cognitive decline among Black Women's Health Study participants. |
| Kotton | 14.0 | Developing Pluripotent Stem Cells to Model and Treat Lung Disease |
| Farrer & Sherva | 13.7 | Genetic Studies of Alzheimer's Disease in Jewish and Arab Populations |
| TCW | 3.9 | Microglia targeted interventions in prodromal Alzheimer's disease stage |
| Goldstein, Mez & Alosco | 3.9 | Validation of Lens Beta-Amyloid as a Novel Biomarker for Early Detection of Alzheimer's Disease at the Boston University Alzheimer's Disease Research |
| Hamburg | 3.7 | Endothelial Cell Health Across the Spectrum of Cardiometabolic Disease |
| Lenburg | 3.2 | Integrating imaging and biopsy-derived molecular markers for the pre-surgical detection of indolent and aggressive early-stage lung adenocarcinoma |
| Wilson | 3.1 | Mechanistic studies of the genetic contribution of desmoplakin to pulmonary fibrosis in alveolar type 2 cells |
| Mizgerd | 3.0 | Fibrin in the Infected Lung |
Foundation awards of note:
- The American Lung Association and LUNGevity Foundation contributed $1 million to Avrum Spira, MD, professor of medicine, pathology and bioinformatics, to intercept lung cancer through immune, imaging, and molecular evaluation.
- The American Cancer Society awarded $792,000 to Jessica Petrick, PhD, MPH, assistant professor of medicine, to study modifiable causes of colorectal cancer in black women
Department of Medicine Announces New Section Chief of Gastroenterology!
The Department of Medicine is delighted to announce that Dr. Christopher S. Huang will become the next Section Chief of Gastroenterology, effective September 1, 2024. Dr. Huang will also be appointed to the Franz J. Ingelfinger, MD Professorship in Gastroenterology. He has served as the interim Section Chief of Gastroenterology since December 2023.
Dr. Huang is a graduate of Cornell University and New Jersey Medical School (now Rutgers Medical School). He completed internal medicine residency at Brigham and Women’s Hospital before joining our training program in gastroenterology in 2001. Dr. Huang joined the BUCAMED faculty in 2004 and was promoted to Clinical Associate Professor of Medicine in 2018. He has served as Boston Medical Center’s Director of Endoscopy Services since 2019.
Dr. Huang has dedicated his career to excellence in patient care and education, with a particular interest in endoscopy education. As a member of the Training Committee of the American Society for Gastrointestinal Endoscopy (ASGE), he taught at and co-directed several national endoscopy courses and co-authored publications on developing core curricula for endoscopic procedures such as colonoscopy, endoscopic ablative techniques, endoluminal stenting, and endoscopic ultrasound.
Dr. Huang is a member of the Alpha Omega Alpha Honor Medical Society and is recognized as a “Top Doctor” by Boston Magazine. He has published numerous review articles and book chapters on inflammatory bowel disease, colorectal cancer screening, and endoscopic and imaging procedures.
Please join us in congratulating Dr. Huang on his new role. He brings tremendous clinical and leadership skills to the Section Chief position, and we are confident in his ability to bring the Gastroenterology Section to new heights in education, research, and clinical care.
DoM STARDoM July Awardees!!
Join us in congratulating this month’s STARDoM awardees, Jean Donald Juillet and Raquel Silveira!
Jean Donald "Don" Juillet
"He makes the clinic run smoothly and always with a smile on his face. He is tireless and will go the extra mile to help our patients. He embodies all that is BMC - care excellence, compassion, and humility."
Job Title: Team Lead ( Medical assistant)
How many years have you been at BUSM/BMC?
5 years
Describe your role within the Department of Medicine:
Aside from doing my Medical Assistant work, I manage and delegate the team's roles and responsibilities to ensure the clinical floor flows properly.
What do you like best about your job?
I appreciate the opportunity to constantly learn & grow.
Favorite thing to do outside of work?
I definitely love spending time with my family asides from watching sports and listening to podcasts…
Raquel Silveira, MBA
"Raquel is an outstanding member of our team who is constantly finding ways to help our team to be our very best."
Job Title: Administrative Manager
How many years have you been at BUSM/BMC?
2.5 years
Describe your role within the Department of Medicine
I like to describe my role as the go-to person for finding the answers and resources that people need. Whether it's information, support, or connections, I am dedicated to helping others by providing the right solutions and tools.
What do you like best about your job?
I take great pleasure in stepping in to assist my colleagues, organizing and supporting them whenever needed. Additionally, I find it immensely rewarding to enhance current processes and procedures, striving to make them more efficient and effective.
Favorite thing to do outside of work?
I cherish spending quality time with my son
Little known fact:
I have dedicated the past 13 years to working in the healthcare field.
DoM Faculty Appointments and Promotions – June 2024
Congratulations to the following Chobanian & Avedisian School of Medicine faculty on their recent promotion.
Associate Professor
Nhan Do, MD, MS, Medicine, specializes in medical bioinformatics focused on effective development and delivery of knowledge tools in the clinical and research workflow. He is the director of the Boston VA Cooperative Studies Program Informatics Center, and he has been instrumental in developing the infrastructure to support research under a learning health system framework, including a large data repository, knowledge repository and software applications to deliver actionable knowledge. One of the informatics center’s projects focuses on improving the efficiency of and facilitating the screening and enrollment of veterans into clinical trials for investigators locally at VA Boston Healthcare System as well as nationally. Prior to joining BU and VA Boston, Dr. Do led the first personal health record for the military and the first health information exchange between the military and its civilian partners at a time when healthcare organizations were reluctant to share data outside of their boundaries. Dr. Do was also the first chief medical information officer to serve on the battlefield to evaluate the health outcomes of military tactics.
Sarah Kimball, MD, Medicine/GIM, specializes in immigration-informed medical care, where she has helped to research and build health systems that are responsive to the needs of immigrant patients. She is the director of the Immigrant & Refugee Health Center at Boston Medical Center, a comprehensive medical home that addresses the barriers that immigrants face to being holistically healthy. Her studies of the critical health care needs of immigrant and refugee health populations have influenced national best practices. For her work in this field, she is known as a national expert in immigrant and refugee health, serving on the board of directors of the Society for Refugee Health Providers and as an associate editor for the Journal of Immigrant and Minority Health. In addition, Dr. Kimball has designed and taught a year-long curriculum for general internal medicine residents focusing on care for immigrant and refugee patients, for which she won a teaching award from the GIM residency office in 2022.
Announcing Chief of Preventive Medicine – Donald M. Lloyd-Jones, MD, ScM
We are pleased to announce that Donald M. Lloyd-Jones, MD, ScM, has accepted the position of director of the Framingham Center for Population and Prevention Science, principal investigator of the Framingham Heart Study, and chief of the section of preventive medicine within the department of medicine at the Chobanian & Avedisian School of Medicine and Boston Medical Center, effective January 1, 2025.
Dr. Lloyd-Jones is the chair of preventive medicine and Eileen M. Foell Professor of Heart Research and professor of preventive medicine, medicine and pediatrics at Northwestern University. He previously served as senior associate dean for clinical and translational research and PI/director of the Northwestern University Clinical and Translational Sciences (NUCATS) Institute from 2012-20. Dr. Lloyd-Jones also served as the national president of the American Heart Association in 2021-22.
He received his BA from Swarthmore College, his MD from Columbia University College of Physicians and Surgeons, and a master of science in epidemiology from Harvard TH Chan School of Public Health. He completed a residency in internal medicine at Massachusetts General Hospital (MGH) and served as chief medical resident. After a cardiology fellowship at MGH, he joined the staff as an attending cardiologist, and was an instructor and then assistant professor of medicine at Harvard Medical School and MGH. He joined the Framingham Heart Study as a research fellow in 1997 and was a research associate from 1999-2004. In 2004, he moved to Northwestern’s Feinberg School of Medicine and became chair of preventive medicine in 2009.
"I am truly excited to return to the Framingham Study and BU, where I began my research career in earnest,” Dr. Lloyd-Jones said. “I am mindful of the incredible legacy of past leaders, who are all giants in our field, like Drs. Dawber, Kannel, Castelli, Wolf and Ramachandran. I am also excited to partner with Drs. Dan Levy, Joanne Murabito, George O'Connor and Emelia Benjamin, who have been ongoing leaders of the Framingham studies for decades. We have an incredible team, and remarkable opportunities to take Framingham and BU to new heights."
“Over decades, the Framingham Heart Study has produced great learnings that further our understanding of cardiovascular disease in America. This transition to new leadership retains the depth of familiarity with the study while advancing the latest science and innovations in epidemiology. We have great confidence in Dr. Lloyd-Jones’ ability to lead the Framingham Heart Study into a new era of scientific excellence,” said David C. Goff, MD, PhD, director of the division of cardiovascular sciences at the National Heart, Lung, and Blood Institute, part of the National Institutes of Health.
Dr. Lloyd-Jones’ research interests include the study of the mechanisms and life course of cardiovascular health and healthy aging, and cardiovascular disease epidemiology, risk estimation and prevention. Other areas of interest include the use of novel biomarkers and imaging of subclinical atherosclerosis to improve prevention, and the epidemiology and outcomes of hypertension and dyslipidemia. His clinical and teaching interests lie in general cardiology, with a focus on prevention.
He also has been a national leader in public health and clinical approaches to promoting cardiovascular health and preventing cardiovascular diseases across the life course. He served as co-chair of the Risk Assessment Guidelines and a member of the Cholesterol Treatment Guidelines Panel for the 2013 ACC/AHA Guidelines for Cardiovascular Disease Risk Reduction; and was the lead member for risk assessment on the 2018 Cholesterol Guidelines Panel and the 2019 Primary Prevention Guidelines Panel. He has authored over 750 peer-reviewed scientific publications and has been a PI or co-investigator on more than 120 grants (the vast majority from NIH).
Dr. Lloyd-Jones has been named a “Highly Cited Researcher” by Clarivate Analytics in each of the last 10 years for being in the top 1% of cited authors in the field of clinical medicine – a distinction that includes only ~420 investigators worldwide.
The recipient of numerous awards and honors, he is a fellow of the American Heart Association, American College of Cardiology and American Society for Preventive Cardiology.
We would like to thank Joanne Murabito, MD, and George O’Connor, PhD, for their valuable contributions and leadership during this interim period. Dr. Murabito will remain co-PI of the Framingham Heart Study.
Please join us in congratulating Dr. Lloyd-Jones and welcoming him to the FHS, BU and BMC.
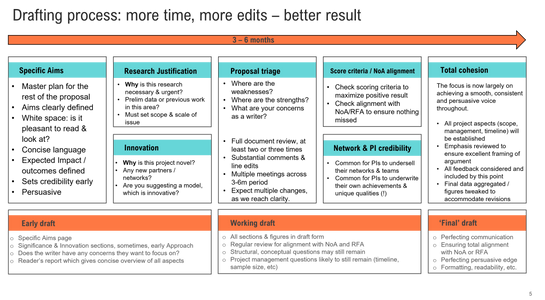
BU DOM Proposal Editing Service | Scott Wilson, Senior Editor
The BU DOM has launched a proposal editing service, with an aim to ensure that our faculty are supported from early draft through to final draft when writing research proposals to prospective sponsors. Through this process, BU DOM hopes to support faculty across all sections as they craft responsive, persuasive, and high quality descriptions of their research potential. A priority area for this service is early- to mid-career investigators (for example, those who are trying to secure RO1s, RO3s, or grants of similar stature). All faculty are welcome and encouraged to engage with this service.
Scott Wilson, senior editor, is available for editing requests by emailing him at sewilson@bu.edu.
Scott has experience and understanding of a wide range of prospective sponsor requirements and RFAs, having worked in research grant management and proposal preparation for European and US sponsors. He can provide consultations with you at every stage of your grant writing process, to help you secure Federal, Foundation, and other types of funding.
How to work with Scott on your research proposal:
- Email Scott at sewilson@bu.edu, with a short description of your request. Please include the deadline you are aiming for!
- Scott will then send you a short questionnaire, which will only take 5 – 10 minutes to complete. This will allow you to include important details about the project that will help Scott tailor his editing to your needs – as well as flag up any concerns you might have with your project.
- Upon receipt of your complete questionnaire, Scott will schedule a call with you. In this first meeting, you and Scott can establish a timeline for your project, discuss unique factors linked to your prospective sponsor (or your project), and touch on any other discussion points you think are relevant to the challenge ahead. It is very common to start with a specific aims page.
- Across a timeline of 3 – 6 months (or perhaps even longer), Scott will work with you on your proposal. You will receive edits and comments that aim to improve your proposal and ensure alignment with the notice of award / requests for applications. Multiple check-in calls can be scheduled as required.
- Prior to your deadline for upload, Scott will help you ensure that your final draft is comprehensive and cohesive and troubleshoot any remaining concerns you may have before you submit your proposal to the sponsor.
Faculty are encouraged to allow 3 – 6 months of time for this process to offer the best value. This means reaching out to Scott early (ideally, at least 3-6 months ahead of your deadline).
We anticipate requests for this service to be high. Scott reports to Dr Salant, Vice-Chair for Research, and manages his portfolio of work accordingly dependent on researcher need & prospective deadline. Although all requests will be considered, priority will be given to those researchers who request the service at least 3 – 6 months ahead of deadline. Should demand be extremely high, a prioritization rubric will be implemented, with details shared to BU DOM faculty in an update.
Message from BU Faculty & Staff Assistance Office for BIPOC Mental Health Awareness Month:
BIPOC Mental Health Awareness Month, observed each July, holds profound significance as it brings critical attention to the mental health challenges uniquely experienced by Black, Indigenous, and People of Color. These communities face systemic racism, discrimination, and historical trauma, which can significantly impact their mental well-being. Recognizing these factors is essential in understanding the full scope of mental health needs within these groups.
The month-long observance underscores the importance of addressing these disparities and advocates for the development and implementation of mental health services that are culturally competent and responsive to the distinct needs of BIPOC individuals.
FSAO is committed to supporting the mental well-being of all our employees, especially acknowledging the unique challenges faced by Black, Indigenous, and People of Color (BIPOC) communities.
How the FSAO Can Help:
- Confidentiality and Support: FSAO counselors provide a safe and confidential space for employees to discuss any personal or work-related concerns they may be experiencing.
- Culturally Competent Approach: At the FSAO, we aim to provide a safe and welcoming space for every employee, honoring and respecting their unique experiences, challenges, and perspectives. Our approach is trauma-informed and culturally responsive, acknowledging the stresses and traumas experienced by those with historically marginalized identities.
- Resources and Referrals: FSAO works with a diverse network of providers who understand the unique challenges faced by BIPOC communities. We can connect employees with additional resources specifically tailored to the needs of BIPOC individuals.
BIPOC Mental Health Month is a great opportunity to prioritize your mental well-being.
Here are some resources and tips:
- BU FSAO BIPOC Mental Health Resources and Self-Care Tips
- Headspace offers meditations led by diverse teachers. Some collection suggestions are: The Shine Collection and Navigating Injustice.
BMC Ranked Top 10 in Nation for Racial Inclusivity
BOSTON – Boston Medical Center (BMC) has been awarded top grades by the Lown Institute, a nonpartisan healthcare think tank, for its achievements and efforts in health equity, clinical excellence, and community collaborations. BMC received an “A” grade for social responsibility, which combined metrics of health equity and value of care alongside patient outcomes, from more than 3,500 U.S. hospitals and 300 health systems nationwide.
BMC’s outreach extends beyond its walls to the neighborhoods it serves. BMC Health System founded its Health Equity Accelerator, an ambitious and aggressive initiative that aims to eliminate the race-based health equity gaps in five clinical areas where major disparities exist including cancer, infectious diseases, chronic conditions, behavioral health, and pregnancy. Additionally, BMC offers programs such as BMC Curbside Care for Moms and Babies to eliminate barriers to care, such as transportation and childcare, by bringing perinatal care right outside their homes. Mothers and babies receive wellness checks, lactation support, and immunization during the first six weeks of life.
BMC also received “A” grades from the Lown Institute for Health Equity, Racial Inclusivity, Inclusivity, Community Benefit, Value of Care, and Avoiding Overuse. In addition, BMC was ranked #1 in Massachusetts for Inclusivity.
“We are honored to be recognized for our work in delivering extraordinary and empathetic solutions that make life healthier and more equitable for the communities we serve,” said Anthony Hollenberg, MD, President of Boston Medical Center. “As an equity-led academic medical center, we are dedicated to pioneering innovative care models and advancing programs that address social determinants of health, designed collaboratively with and for our patients and communities."
“Great care is only great if everyone can access it,” said Vikas Saini, MD, president of the Lown Institute. “We need hospitals that are not only leaders in clinical care, but also strong community partners —and these socially responsible hospitals are showing the way.”
In the fifth annual rankings, the 2024-25 Lown Index evaluates hospitals on over 50 measures including novel metrics such as community benefit, racial inclusivity, and avoidance of overuse. Data sources include Medicare fee-for-service and Medicare Advantage claims, CMS patient safety data and hospital cost reports, and IRS 990 forms, among others. Full methodology can be found on the Lown Index website.