Reducing Readmissions for Patients with Heart Failure and COPD
While BMC’s all cause 30-day readmission rate was 10.96% in FY17, certain populations had much higher readmission rates particularly heart failure (HF) (23.73% FY17) and COPD (24.81% FY17).
With almost 1 in 5 HF and COPD patients readmitted, reducing readmissions for these patients has become an important hospital and quality priority.
Multidisciplinary pilots focusing on transitions of care started on 7/5/18 on E7N for patients with HF, with full go-live anticipated by February 2019. Menino 6 is piloting similar strategies for patients with COPD. Both pilots include:
- Adoption of “Teach Back” methodology for all patient teaching
- Partnering with home care providers such as our VNAs for home med reconciliation
Unique to HF:
- HF consult triggers for patients on non-cardiology teams
- Standardization of patient instructions in AVS using smart phases for HF
- Facilitated early discharge transitions of care (TCM) appointments
- Personalized reminder calls by Cardiology Clinic staff one day before post discharge appointments for patients with HF
Unique to COPD:
- Inpatient COPD NP consult with follow up outpatient appointment. Welcome Alexis Gallardo Foreman, NP to the COPD care team! Alexis is available to see patients with COPD in both the inpatient and ambulatory settings.
During the 8-week HF pilot on E7N, the 30d readmission rate decreased from 21.6% to 12.9%., with most reduction seen in the 7-10d readmission rate. In Jan-Nov 2018, COPD readmission rate was 20.7%.
You are the critical link to connecting our patients with HF and COPD to these proven strategies for reducing readmission and improving health. Please consult the HF or the COPD service to activate patient care resources!
Resident QI Corner – Winter ’19
Managing discharge from Inpatient Heme/Onc Service
The inpatient Hematology/Oncology team at BMC is a busy service full of patients with complex medical problems and diverse pathologies requiring intricate care plans. Thus, discharges from the Heme/Onc inpatient service are complicated and are often derailed by unforeseen variables.
We sought to increase the safety and timeliness of discharges by implementing a standardized approach to discharge planning starting on the day of admission. We designed a discharge time-out checklist for the Heme/Onc team. The team can run the checklist prior to a patient being discharged to ensure all important aspects are addressed. A Heme/Onc Bundle was also created to be used with each daily note to keep up to date on discharge planning.
We implemented the checklists as SmartPhrases from November 2017 to February 2018 and compared to pre-intervention data over the same months from 2016- 2017. After our intervention implementation, discharge time of day on the service improved by 13 minutes and time of discharge order placement improved by 39 minutes. On average, the Heme/Onc bundle was used in 86% of notes. Future directions include use of a standardized discharge summary template for the Heme/Onc service to help facilitate safe transitions of care.
By Rani Chudasama, MD and Matt Strickland, MD


IHI Conference 2018 - Dec 9 - 12
Quality Improvement Patient Safety (QIPS) pathway IM residents attending IHI 2018 National Forum:
Swetha Ramachandran, MD - Improving Inter-Hospital Transfers Through Implementation of a Transfer Accept Note
Calan Sowa , MD & Ruchika Sangani, MD - Improving Primary Care Follow-Up through In-Person, In-Hospital Appointment Negotiation
 Nancy Desai, MD - Cervical Cancer Screening and Prevention in Patients with Systemic Lupus Erythematosus
Nancy Desai, MD - Cervical Cancer Screening and Prevention in Patients with Systemic Lupus Erythematosus
 Kristin Hlebowitsh , MD - Minimizing Isolation: Re-screening inpatients for MRSA infection
Kristin Hlebowitsh , MD - Minimizing Isolation: Re-screening inpatients for MRSA infection
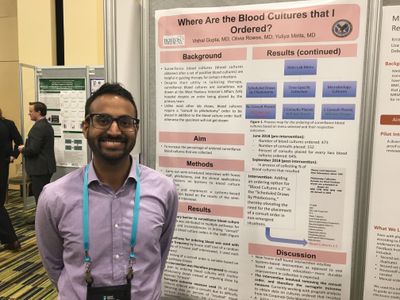 Vishal Gupta , MD- Where Are the Blood Cultures that I Ordered?
Vishal Gupta , MD- Where Are the Blood Cultures that I Ordered?
Kris Clark, MD and Shaleen Chakyayil , MD - EMR-Based Intervention to Improve Venous Thromboembolism (VTE) Risk Assessment and Prescribing Practices
Other QIPS residents in attendance:
Mangwe Sabtala, MD
Prianka Ballal, MD
Laura Chiu, MD
Olivia Rowse, MD
For those of us attending for the first time, we got our batteries charged! We look forward to continuing to bring positive change to our patients and to our community.
Reducing Catheter Associated Urinary Tract Infections (CAUTI)
The CAUTI rate on the wards and ICUs for FY18 YTD was 25 infections with a goal of ZERO (FY17, there were 25 infections).
Please only place indwelling urinary catheters for:
- Hourly urine output monitoring (only in the ICUs)
- Management of urinary retention, and
- Assistance in healing a stage 3 or 4 pressure ulcer
If a patient has a fever with a Foley catheter in place, DO NO SEND BOTH A URINALYSIS AND A URINE CULTURE TOGETHER! First send a urinalysis (UA). If the UA is positive (greater than 10 WBC, presence of bacteria as shown by bacteria on microscope slide, positive leukocyte esterase, or positive nitrates), have the nurse change the Foley catheter and then send a urine culture. This helps greatly reduce false positive urine cultures which are then labeled as CAUTIs. There is now a BPA which fires as a reminder to adhere to this process.
Always remove Foley catheters as soon as they are no longer needed; review need for placement as DAILY rounds and Multidisciplinary Rounds.
Reducing Clostridium Difficile Infections
One major component of preventable harm is hospital-acquired C. difficile infections. Due to the ongoing work of Deb Gregson and the QI team, we have made considerable progress. BMC is above goal with FY18 Standardized Infection Ratio (SIR) of 0.97 (goal ≤0.7).
Key drivers for reducing C diff. are decreasing unnecessary testing, ensuring timely isolation/contact precaution adherence, antibiotic stewardship, and washing hands with soap and water. Ways to help:
- Do not send C diff. test unless > 3 loose or watery stools in a 24 hour period.
- Do not retest within 7 days of a previous negative, within 30 days of a previous positive C diff. test result, or if the patient has had a positive result within the current admission (prior results will be made available when order placed).
- No need to test for cure
- BPA will alert you if the patient has received laxatives in past 48 hours.
- If you have a suspicion for C diff., place Contact PLUS Isolation Precautions which is part of the C diff. test order.
- Whenever you enter a patient’s room on Contact PLUS, Wash in, Gown up, Glove up. Dispose of dress in room and SOAP OUT.
- Discontinue precautions if test is negative.
- Use oral vancomycin as first line treatment for C diff. (thought to have more rapid response than metronidazole and reduce contagion more quickly.)
2018 BACO MassHealth PC Group Quality Bonus Program
Starting in 2018, MA Executive Office for Health and Human Services will generate a Quality Score for each ACO participating in the new MassHealth ACO program. This Quality Score will determine our ACOs share of any surplus or deficit accrued. The amount of surplus or deficit will be based on the difference between our ACO’s state-assigned spending budget and the actual total cost of care for the patients attributed to BACO.
The state’s Quality Score will be based on both claims-based data and our submission to MassHealth of chart-based information. In Performance Year 1 (2018), to receive a quality score of 100%, our ACO is only required to submit all requested data (referred to as “pay for reporting”). Beginning in 2019, our score will be based on our performance on the various metrics, making it essential that BACO begins to build infrastructure across the ACO to enable optimal metric performance.
The amount of the Primary Care Group Quality Bonus, tied to $2 per member per month, awarded to each group will be determined by the group’s performance in three distinct areas:
- Complete submission of requested MassHealth beneficiary clinical data to BACO to enable successful BACO pay for reporting in 2018.
- Performance by the group on a BACO-created Ambulatory Visit Quality Metric, which is success in maximizing the number of BACO patients seen in the ambulatory setting. Only 60% of BACO patients were seen between 3/1/17 and 12/31/17.
- Performance by the group in the BACO-created Diagnosis Identification Program Screening for homelessness and depression which can be performed by any office staff. Based upon historical performance, that screening rates of 80% are feasible for both homelessness and depression. The bonus, however, will be based upon each group’s performance normalized to the BACK mean performance rate. Screening for homelessness should be done as part of a larger social determinants of health screen using a screening tool such as THRIVE. Screening for depression should be done with a screening tool such as PHQ2 or 9. Groups should make every effort to capture an appropriate diagnosis code with appropriate documentation in the medical record whenever a screen yields a diagnosis (e.g. homeless or major depressive disorder). Groups should also ensure that positive screens are addressed by clinical providers during the encounter to ensure appropriate care of patients.
If you would like more details about the BACO MassHealth Primary Care Group Quality Bonus or any of the metrics, please contact Dr. Brian Jacobson at brian.jacobson@bmc.org.
BMC Quality Goals FY 19
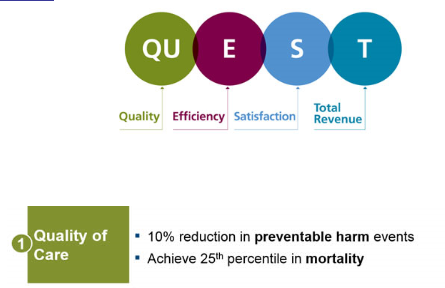
1. 10% reduction in preventable harm events. The Preventable Harm Index includes 16 Hospital-Acquired Conditions (HACs), such as clostridium difficile infections, central line associated bloodstream infections (CLABSI) and catheter associated urinary tract infections (CAUTI), and Patient Safety Indicators that are tied to external reputation and reimbursement. BMC is predicted to meet goal for Preventable Harm Index Observed/Expected for FY18 <0.90, representing a 10-15% reduction in events from FY17. FY19 goal will be < 0.90.
2. Achieve top 25th percentile nationally in mortality with an Observed/Expected (O/E) mortality ratio of <0.845. BMC FY18 met goal at 0.789.
BMC Physician Quality Leaders
In July 2016, BMC reorganized the Physician Quality Leaders, funding fewer quality leaders but giving each more responsibility and time to actually get things done. They report to Dr. James Moses, BMC Chief Quality Officer, and address patient safety events as well as promote hospital quality initiatives. They are also tasked specifically to work with residents and help mentor resident projects and ideas!! Faculty and housestaff, please reach out to the physician Quality Leader or the Medical Directors in your area of interest. The current physician Quality Leaders are:
- Chris Andry, PhD — Lab and Pathology
- Willie Baker, MD — Emergency Medicine
- Glenn Barest, MD — Radiology
- Lisa Caruso, MD, MPH — Medicine (including Family Medicine, Neurology, Psychiatry, and all subspecialties)
- Ron Iverson, MD, MPH — Obstetrics/Gynecology
- Bernadette Levesque, MD — Pediatrics
- David McAneny, MD — Surgery (including all subspecialties)
- Juhee McDougal, MD — General Internal Medicine, Ambulatory
- James Murphy, MD — Critical Care (MICU, SICU, CCU), Medical Director of Inpatient Quality
- Lauren Nentwich, MD — Emergency Medicine
- Susan O'Horo, MD — Interventional Radiology
- Susannah Rowe, MD, MPH — Ophthalmology
Hem/Onc Section Partners with Bristol-Myers Squibb for Cancer Research
Street Insider publishes article "Bristol-Myers Squibb (BMY) Announces Research Collaboration with Boston Medical Center to Investigate Markers of Immuno-Oncology Response & Resistance"
The hematology/oncology section at Boston Medical Center is partnering with Bristol-Meyers Squibb to investigate biomarkers in a variety of cancers to predict Immuno-Oncology I-O responses.
"We look forward to partnering with Bristol-Myers Squibb on this study to identify and assess biomarkers across a diverse patient population, providing us with a deeper and more comprehensive understanding of I-O resistance.” - Dr. Matt Kulke, BMC Chief of Hematology/Oncology Section
Discovery of the Month: Dec 2018
"Retinoic Acid Signaling is Essential for Airway Smooth Muscle Homeostasis"
Presented by Dr. Chen at Grand Rounds, December 14, 2018
This is the first installment in the Dept of Medicine series, Discovery of the Month. Recent projects are recognized and featured during a special monthly grand rounds for significant findings and publications.
Elevated Blood Pressure in People Under 40 Poses Hazard of Developing Cardiovascular Diseases Prematurely
High blood pressure or hypertension is a major health problem that affects more than 100 million people in the U.S. (using the current 130 systolic or 80 diastolic) and over one billion worldwide. Despite being considered a disease of older adults, there are two new studies in the Journal of the American Medical Association (JAMA) that are reporting the association of high blood pressure with the risk of premature cardiovascular disease (CVD) in adults younger than 40. In an accompanying JAMA editorial, Vasan Ramachandran, MD, FACC, Professor of Medicine in the Department of Medicine, mentions that major gaps exist in the current knowledge regarding the epidemiology, diagnosis, risk stratification and management of higher blood pressure levels in young adults.
 Felicia Chen,
Felicia Chen,