Caring for the Transgender Patient
Caring for the Transgender Patient: Grand Rounds Discussion From Beth Israel Deaconess Medical Center
By Howard Libman, MD; Joshua D. Safer, MD; Jennifer R. Siegel, MD; Eileen E. Reynolds, MD
 In a recent Medical Grand Rounds at Beth Israel Deaconess Medical Center, Boston area leaders in care for transgender patients, including Jenny Siegel, MD, Assistant Professor of Medicine at Boston University School of Medicine, and Medical Director of the Center for Transgender Medicine and Surgery at Boston Medical Center, discuss critical components of the clinical guidelines for gender affirming hormones and surgery.
In a recent Medical Grand Rounds at Beth Israel Deaconess Medical Center, Boston area leaders in care for transgender patients, including Jenny Siegel, MD, Assistant Professor of Medicine at Boston University School of Medicine, and Medical Director of the Center for Transgender Medicine and Surgery at Boston Medical Center, discuss critical components of the clinical guidelines for gender affirming hormones and surgery.
Clinical Guidelines
In the article, the following questions are posed to the panel of experts to discuss care guidelines in general and as they relate to the story of a particular patient considering gender-affirming care.
Conclusions
DOM Faculty Named 2020 Boston “Top Docs”
44 faculty members of the Department of Medicine have been named to Boston Magazine's annual Top Docs List.

Cardiac Electrophysiology
Robert Helm
Kevin Monahan
Cardiovascular Disease
Eric Awtry
Gary Balady
Sheilah Bernard
Robert Eberhardt
Alice Jacobs
Endocrinology, Diabetes
& Metabolism
Sonia Ananthakrishnan
Alan Farwell
Michael Holick
Stephanie Lee
Elizabeth Pearce
Gastroenterology
Charles Bliss
David Lichtenstein
Robert Lowe
David Nunes
Geriatric Medicine
Heidi Auerbach
Lisa Caruso
Hollis Day
Hematology
Vaishali Sanchorawala
Internal Medicine
Thomas Barber
Melissa DiPetrillo
Warren Hershman
Angela Jackson
Susan Phillips
Jeffrey Samet
Charles Tifft
Medical Oncology
Gretchen Gignac
Kevan Hartshorn
Matthew Kulke
Adam Lerner
Nephrology
Laurence Beck
Jasvinder Bhatia
Lauren Stern
Pulmonary Disease
John Berk
Jeffrey Berman
John Bernardo
Elizabeth Klings
Frederic Little
George O’Connor
Arthur Theodore
Rheumatology
David Felson
Eugene Kissin
Robert Simms
Will Massachusetts Ban Flavored Tobacco?
Dr. Hasmeena Kathuria, Associate Professor of Medicine in the Section of Pulmonary, Allergy and Sleep Medicine and director of the Tobacco Treatment Center at Boston Medical Center, joins State Sen. John Keenan on Radio Boston to discuss the future of a flavored tobacco ban now before the Massachusetts Senate. The proposal passed in the state's House of Representatives last week.
| Listen to the Full Segment Here |
Dr. David Coleman to Receive Distinguished Chair of Medicine Award
 Dr. David Coleman, Wade Professor and Chairman of Medicine, has been named the 2020 recipient of The Robert H. Williams, MD, Distinguished Chair of Medicine Award, presented by the Association of Professors of Medicine (APM).
Dr. David Coleman, Wade Professor and Chairman of Medicine, has been named the 2020 recipient of The Robert H. Williams, MD, Distinguished Chair of Medicine Award, presented by the Association of Professors of Medicine (APM).
From the Alliance for Academic Internal Medicine Announcement:
"Described as an “outstanding chair who has distinguished himself through service to his department and the academic internal medicine community,” Dr. Coleman’s “impact and reach are exceptional and his contributions to the tripartite missions of our profession – education, clinical care, and research – are extraordinary.” Examples of Dr. Coleman’s vision, systems thinking, and ability to lead change abound: from his passion for “providing exceptional clinical care despite the many impediments posed by social determinants of health” to his commitment to “placing the Department at the forefront of new and evolving research initiatives” to serving as “a champion for education, mentorship, faculty development, and diversity.” His dean notes that “he is one of my most trusted senior leaders; someone to whom I can turn for his innovative approaches to interdisciplinary collaborations and medical student education.”
Dr. Coleman has served as Chair of Medicine at Boston University School of Medicine and physician-in-chief at Boston Medical Center since 2006. During his tenure, the Department has seen tremendous growth in its research and clinical care portfolios and educational programming.
| Read More |
Dr. Weining Lu Named BU Innovator of the Year
 Dr. Weining Lu, associate professor in the section of Nephrology, has been named 2019 BU Innovator of the Year.
Dr. Weining Lu, associate professor in the section of Nephrology, has been named 2019 BU Innovator of the Year.
Dr. Lu's research focuses on the gene ROBO2 as it relates to a kidney’s filtering ability, and has led to a collaboration with Pfizer’s Centers for Therapeutic Innovation (CTI) since November 2012.
This unique collaboration between academia and industry on developing mechanisms to affect ROBO2 function in adults will have far reaching impacts on the 37 million people in the US and 850 million people worldwide with chronic kidney disease.
| Read Full Article in the Brink |
Removing Unnecessary Contact Isolation Precautions
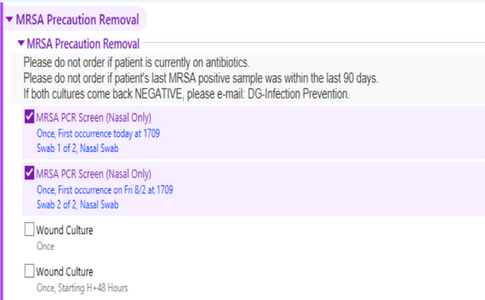 Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium that can be transmitted via skin-to-skin contact and may cause severe infections. BMC has a policy to place MRSA-colonized patients on contact isolation precautions. An estimated 15-30% of colonized patients clear within 90 days giving us the opportunity to reduce the need for private rooms, improve staff and patient satisfaction by reducing need for protective gear, minimize “isolation precaution fatigue”, and save an estimated $6.4 million/year by removing unnecessary MRSA precautions.
Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium that can be transmitted via skin-to-skin contact and may cause severe infections. BMC has a policy to place MRSA-colonized patients on contact isolation precautions. An estimated 15-30% of colonized patients clear within 90 days giving us the opportunity to reduce the need for private rooms, improve staff and patient satisfaction by reducing need for protective gear, minimize “isolation precaution fatigue”, and save an estimated $6.4 million/year by removing unnecessary MRSA precautions.
Eligible MRSA positive adults for rescreening are those:
- With no positive MRSA PCR or culture in the prior 90 days, and
- Who do not have an active antibiotic order.
A Best Practice Advisory Logic has been introduced to Admission Order Sets to facilitate removal MRSA precautions in eligible patients. This logic looks at patients previously identified as MRSA positive to begin a re-screening process at admission. The order is two-step testing, once on the day of the order and the second 48 hrs later if the first test is negative.
If both screens/cultures come back negative, please e-mail DG-Infection Prevention and isolation precautions will be removed.
PLEASE ONLY DE-SELECT ORDERS if patient is currently on antibiotics.
Resident Corner Fall ’19
STARS Candy Rounds by Swetha Ramachandran, MD and the QIPS Residents
As part of the internal medicine residency program at BMC, there is a Quality Improvement and Patient Safety (QIPS) pathway for residents who are interested in identifying patient safety issues and improving outcomes using quality improvement methodologies. This year the residents in the QIPS pathway are working to promote resident participation in quality improvement initiatives.
To achieve this goal, we have started weekly patient safety rounds where a QIPS resident will touch base with medicine teams in person to inquire about patient safety issues that the teams have encountered in the hospital. With these weekly rounds, we hope to increase resident STARS reporting and patient safety awareness.
Additionally, each week a STARS report will be reviewed by a QIPS resident with the aim of improving recurrent systems issues as well as providing feedback to the reporting provider. As a group, the QIPS pathwa
y residents are excited and motivated to make changes that will improve patient care and streamline hospital processes.
BMC Joins the Age-Friendly Health System Community
To better support older adults and improve their health outcomes, health systems must put in place comprehensive, coordinated evidenced-based models that better deliver care to the growing aging population.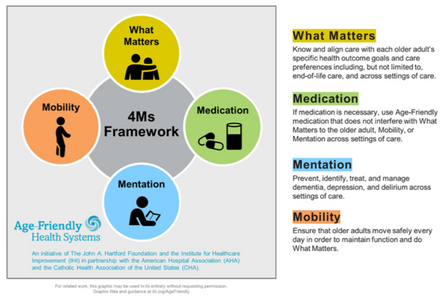
In September 2018, BMC joined John A. Hartford Foundation-Institute for Healthcare Improvement’s (IHI) Age-Friendly Health System Community in spreading age-friendly care with the goal of reaching 1,000 US hospitals and 1,000 medical practices by December 2020.
BMC is working towards a comprehensive approach to implementing best practices under the 4Ms (What Matters, Medication, Mentation, and Mobility) for each patient 65+ admitted to the hospital.
BMC is well on its way to becoming an Age-Friendly Health System!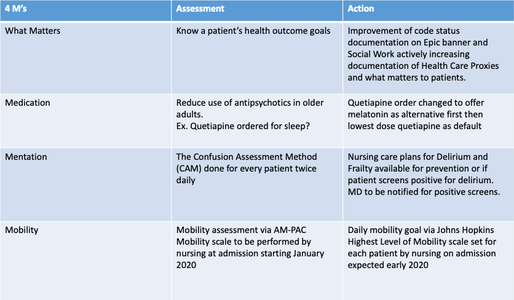
Success of New Hyperglycemia Crisis Management Guideline
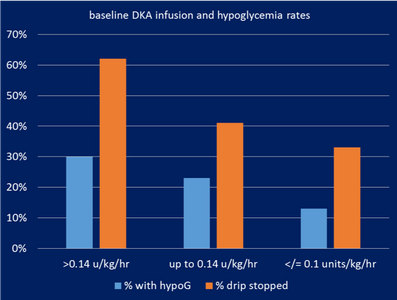
In AY2018 the Endocrine Subcommittee of the Pharmacy and Therapeutics Committee rolled out changes to the longstanding BMC Hyperglycemic Crisis Management Guideline, which had been in use for more than a decade. A QI project done the prior year had shown higher rates of hypoglycemia (blood glucose (BG) <70) in patients after up-titration of the insulin infusion drip, in particular to doses of >0.14 unit/kg/hour of insulin. These patients had a 3-fold higher rate of hypoglycemia, and in 60% of patients treated at this dose needed to have the drip stopped to prevent hypoglycemia (Figure 1).
Led by Dr. Sara Alexanian the Director of Inpatient Diabetes Program and Quality Leader in the Section of Endocrinology, a multidisciplinary group including en
docrine, pharmacy, nursing and IT came together to create an updated guideline. The process included reviewing primary literature supporting current hyperglycemic crisis management, review of national standards as well as protocols at outside institutions. Based on this review a new guideline was developed. Major changes included:
- Removal of default increases in the insulin infusion rate, and
- An updated insulin titration algorithm based on solid published evidence.
Subsequently there were several months of ED and ICU nursing education, including - in-services by endocrine and pharmacy, as well as a required Health Stream course. The new guideline was rolled out in September 2019.
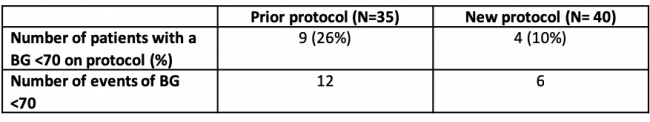
Three months after the release of the new guideline, a chart review was done on the 40 patients who were treated with the new algorithm compared to 35 patients on the prior protocol. There was a 60% reduction in hypoglycemia (26% on the prior protocol down to 10% on the new protocol, Table 1). Furthermore the total episodes of hypoglycemia decreased with the new protocol, as did the number of times the drip needed to be stopped to prevent hypoglycemia. Further analysis showed that despite the lower rates of hypoglycemia, there was no significant increase in the time to DKA resolution.
The multidisciplinary workgroup continues to engage with nursing to improve the guideline. Based on feedback, new changes include making minor adjustments to the insulin titration algorithm and making the transition to dextrose-containing fluids a default in the order set to ease nursing work-flow. Furthermore, when substantial discrepancies occur between the ED and ICU weights, the nurse will be prompted to adjust the infusion dose appropriately for weight obtained on admission to the ICU. These changes are expected to go live in the fall 2019 with the hope of reducing hypoglycemic events further!
BMC Quality Goals for Fiscal Year 2020 (FY 20)
Reducing Preventable Harm Index (PHI)
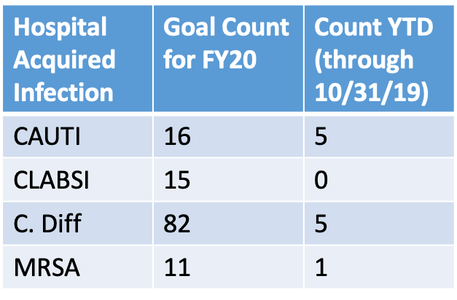
PHI is comprised of the 4 major Hospital Acquired Infections (HAIs) with a goal of 1.0 (YTD 0.84):
- Catheter associated urinary tract infection (CAUTI),
- Central Line Associated Bloodstream Infections (CLASBI)
- Hospital acquired Clostridium difficile infections (CDIFF) and
- Methacillin-Resistant Staph aureus bacteremia
The PHI also contains several perioperative/periprocedural complications and “never events” such as falls, pressure ulcers, and iatrogenic pneumothorax. The post-procedural complications followed most closely in internal medicine are venous thromboembolic events, hemorrhage/hematoma and development of acute kidney injury.
This year marks a major change in BMC’s approach to the monitoring and goal setting for HAIs . We are shifting from rates and standardized infection ratios to simply following counts as we try to “chase zero” with the goal of zero events for each floor team. Following infection counts will allow us to assess and respond more quickly as an organization. Goal counts are in the table below.
If your team is following a patient who develops an HAI, please respond to the nurse manager’s request to meet to assist in the preparation of a preventability analysis.
Reducing Mortality
- BMC’s O/E (Observed to Expected) mortality for FY2019 was 0.79 below the goal of <0.84.
- BMC’s O/E Mortality Goal for FY2020 is 0.77 which places BMC in the top 25th percentile nationally in mortality compared to other academic medical centers.
- What can I do?
- Capture severity of illness by documenting all significant conditions in the H&P.
- Engage Serious Illness Support Services for patients who have been identified as being at high risk of mortality in the next 6 months for discussions on advance care planning.
- Refer BMC patients who are Comfort Measures Only patients for inpatient hospice screening.