2025 Evans Days Speakers and Schedule Announced!!!!!
Thursday, October 16
8:15am - 9:15am Oral Presentations | L110
9:30am– 11:00am Basic Science Poster Presentations | Hiebert Lounge
11:15am – 12:45pm Basic Science & Clinical Research Poster Presentations | Hiebert Lounge
1:00pm – 1:30pm DoM Chair of Medicine Interviews Dr. Humpreys | Keefer Auditorium
1:30pm - 2:30pm ARC & D. Coleman Prize Presentations | Keefer Auditorium
2:30pm-3:00pm Coleman Award Recipient Meet & Greet | Keefer Auditorium
3:00pm-4:00pm Wilkins Visiting Professor Lecture | Keefer Auditorium
5:30pm - 8:30pm Reception & Awards Ceremony | Hiebert Lounge
Wilkins Professor
Benjamin D. Humphreys, MD, PhD
Joseph Friedman Professor of Renal Diseases in Medicine
Chief, Division of Nephrology
Washington University
Friday, October 17
12:00pm – 1:00pm Ingelfinger Visiting Professor Lecture | Keefer Auditorium
Ingelfinger Professor
Jean S. Kutner, MD, MSPH
Chief Medical Officer, University of Colorado Hospital
Chief Academic Officer, UCHealth
Distinguished Professor of Medicine and Associate Dean for Clinical Affairs
University of Colorado School of Medicine
2025 DoM DEIA Pilot Grant Awardees!!
The Department of Medicine launched its inaugural Diversity, Equity, Inclusion, and Accessibility (DEIA) Pilot Grant program this year, supporting innovative projects led by interdisciplinary teams of faculty, trainees, and staff. Proposals focused on improving clinical care, education, workforce development, community engagement, and research to advance DEIA across the department.
The first annual DEIA Pilot Grant recipients are:
Jessica Fetterman, PhD (Vascular Biology): Tissue is the Issue: Exploring Barriers and Facilitators to Postmortem Organ Donation for Research to Diversify Cardiac Biobanks. A proposed study to understand limited representation of historically marginalized racial/ethnic groups in postmortem organ biobanks. They plan to use surveys and town halls including Framingham Heart Study and BMC patients to achieve this goal. Team members include Deepa M. Gopal, MD, MS, Jesse D. Moreira-Bouchard, PhD, Zachary Milstone, MD, PhD, Anna Zhebrun, Joshua Lepson, Karen Li, Jason Cunha, MS, Nathanial Fisher, MS, Anjali Anilkumar, Hahnbie Kim, Cosette Giroux, and Zoe Trainer.
Elliot Hagedorn, PhD (Hematology & Oncology): Reaching Further with the BU-BMC Summer Science Scholars Outreach Program. The team proposes to expand an existing high school research training program to include more longitudinal mentoring, cohort collaboration, shadowing, and peer/alumni engagement. Co-directors are Dr. Gwen Beacham and Zewde Ingram.
Lucy Schulson, MD, MPH (GIM): IMPACT-IRHC: Implementation of MedAction Plan in BMC’s Resident Immigrant and Refugee Health Clinic. A proposed pilot the implementation of a multi-lingual transitions of care document written at a 5th grade reading level (MedAction Plan) in BMC primary care clinics after adapting it for BMC immigrant/refugee patients. Co-investigators are Drs. Sarah Kimball and Kirsten Austad.
Join us in congratulating the DEIA Pilot Grant awardees!!
DoM Research Award Recipients!
The Department of Medicine proudly recognizes the recipients of its inaugural Research Awards for their outstanding contributions to scientific discovery and innovation. Their dedication and passion have not only advanced their respective fields but have also enriched the community and set a high standard for future research excellence.
Research Excellence Awards
- Valerie Gouon-Evans, PharmD, PhD
- Vaishali Sanchorawala, MD
Early Career Research Award
- Titilayo Ilori, MD, MSc
Interdisciplinary Research Awards
- Elizabeth Klings, MD
- Mari-Lynn Drainoni, PhD, MEd
Research Excellence Society
- Hussein Assi, MD
- Ruben Dries, PhD
- Christopher Heaphy, PhD
- Elliott Hagedorn, PhD
- Jeffrey Samet, MD, MA, MPH
- Carl Streed, MD, MPH, FACP
- Gustavo Mostoslavsky, MD, PhD
- Kim Vanuytsel, PhD
Congratulations to all the awardees!
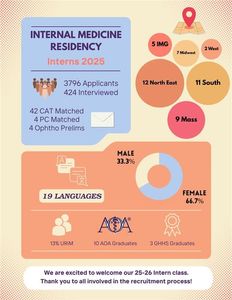
Incoming Interns for Class of 2028!
The Department of Medicine is excited to share the results of this year’s NRMP residency match. It has successfully matched an outstanding class of well-rounded individuals who will be joining for the upcoming academic year. As shown in the graphic below, the department has attracted a diverse cohort of talented individuals from across the country and around the world.
A sincere thank you goes to the faculty for their support throughout this recruitment season. Their involvement plays a vital role in attracting the best and brightest to join BMC.
Click here to see the 2025-2026 Intern Class!
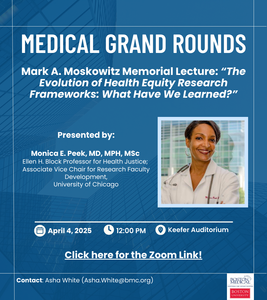
Mark A. Moskowitz Annual Memorial General Internal Medicine Grand Rounds Lecture
2025 DoM DEIA Week Recap!
The Department of Medicine’s annual Diversity, Equity, Inclusion, and Accessibility (DEIA) Week brought together faculty, staff, trainees, and community members for a series of engaging and impactful events from March 10-14.
Monday, March 10
Poster Showcase + Oral Presentations
Hiebert Lounge | 10:30 AM - 1:30 PM
The week kicked off with an inspiring showcase of DEIA-focused research, education, programming, and patient care initiatives. Faculty, staff, and trainees presented their posters highlighting ongoing efforts to advance equity in medicine. The morning featured oral presentations, providing attendees with deeper insights into innovative DEIA projects.


Tuesday, March 11
Panel Discussion: Molding a Culture – Turning Intention into Action
Hiebert Lounge | 8:00 AM - 10:30 AM
Tuesday’s event emphasized transforming DEIA goals into concrete actions. A distinguished panel discussed strategies for fostering inclusive workplace environments, leadership development, and community engagement. Attendees participated in breakout discussions, brainstorming three actionable ways to integrate DEIA principles into daily life and forming new collaborations to drive change.

Wednesday, March 12
Wellness Wednesday
Evans Conference Rooms | 11:00 AM - 3:00 PM
Midweek, participants took a moment to focus on well-being through a variety of wellness-centered activities. Highlights included:
- Virtual Workshop: Managing Change and Uncertainty with BU FSAO
- Food & Nutrition Pre-ARC Lunch: “Food as a Unifier & Cultural Humility”
- Acupuncture Sessions
- Puppies & Lunch!
- Learn to Make Paper Cranes with Mike Galatis
Thursday, March 13
DEIA Week Celebration
Hiebert Lounge | 4:30 PM - 6:30 PM
Attendees gathered for an evening of art, food, drinks, and camaraderie, celebrating the department’s commitment to diversity and inclusion.

Friday, March 14
Grand Rounds: Conversations on Accessibility
Keefer Auditorium | 12:00 PM - 1:00 PM
The week concluded with a compelling Grand Rounds presentation by Dr. Lisa I. Iezzoni, Professor of Medicine at Harvard Medical School. Dr. Iezzoni’s talk, Conversations on Accessibility, shed light on critical issues related to accessibility in healthcare and academia, inspiring attendees to advocate for more inclusive practices.

We look forward to continuing these important conversations and initiatives in the future. Thank you to everyone who participated and helped make DEIA Week a success!
Thriving Together: Advancing Health, Cultivating Leaders and Collaborating on Community Solutions | April 25, 2025
Thriving Together: Advancing Health, Cultivating Leaders and Collaborating on Community Solutions
Friday, April 25, 2025
On April 25, 2025, the inaugural “Thriving Together: Advancing Health, Cultivating Leaders and Collaborating on Community Solutions,” will bring together a group of deeply committed community partners and emerging health professional leaders. We will share best practices and cement our collaborations for the future of improving community health and health care access in the Greater Boston Area.
The Summit is being hosted by the Boston University Chobanian & Avedisian School of Medicine, Boston Medical Center, and People Power Health.
Summit Goals:
- Create a shared platform for trainees and early-career professionals across disciplines (including but not limited to medicine, nursing, public health), and community-based organizations (CBOs) in the Greater Boston Area to share best practices for closing health gaps in the community (advocacy, education, research, health care innovation) through talks, poster presentations and relationship building.
- Foster sustainable and enduring connection and collaboration between future health professionals and CBOs who wish to work together to advance health for the Greater Boston Area.
- Support the work of future health professionals and CBOs by providing networking and funding opportunities.
When: Friday, April 25, 2025 8:00 am - 5:00 pm.
8:00 am - 1:00 pm
Morning workshops, community power activities and analysis, relationship building, and lunch.
1:00 pm - 3:30 pm
Afternoon networking activities, panel discussions, topical breakout sessions, and emerging leaders and community partners spotlights.
3:30 pm - 5:00 pm
A culminating poster session highlighting completed projects and works in progress that demonstrate successful activities in promotion of health in the Greater Boston Area.
Where: Hiebert Lounge, at Boston University Medical Campus, 72 E Concord St, Boston, MA
Who: Attendees include trainees and early-career professionals across disciplines (including but not limited to medicine, nursing, public health, social work, pharmacy, etc), community partners, public and private sector collaborators, with a shared commitment to improving health for communities in the Greater Boston Area.
DoM Top Docs 2025
We are excited to announce this year's DoM top docs! Learn more here.
Cardiology
Gary J. Balady, MD
Sheilah A. Bernard, MD
Robert T. Eberhardt, MD
Omar K. Siddiqi, MD
Claudia P. Hochberg, MD
Anthony D. Litvak, MD
Ashvin N. Pande, MD
Endocrinology, Diabetes & Metabolism
Sara M. Alexanian, MD
Sonia Ananthakrishnan, MD
Beth M. Cohen, MD
Alan P. Farwell, MD
Shirin Haddady, MD, MPH
Stephanie L. Lee, MD, PhD
Elizabeth N. Pearce, MD
Gastroenterology
Christopher S. Huang, MD
David R. Lichtenstein, MD
Robert C. Lowe, MD
David P. Nunes, MD
Geriatrics
Heidi P. Auerbach, MD
Lisa B. Caruso, MD
Hollis D. Day, MD, MS, MHPE
Won M. Lee, MD
Hematology & Medical Oncology
Gretchen A. Gignac, MD
Matthew Kulke, MD
Adam Lerner, MD
Vaishali Sanchorawala, MD
J. Mark Sloan, MD
Infectious Disease
Carlos J. Acuna-Villaorduna, MD
Sabrina A. Assoumou, MD, MPH
General Internal Medicine
Melissa D. DiPetrillo, MD
Warren Y. Hershman, MD, MPH
Angela H. Jackson, MD
Susan L. Phillips, MD
Jeffrey H. Samet, MD, MA, MPH
Carl G. Streed, MD, MPH, FACP
Charles P. Tifft, MD
Nephrology
Laurence H. Beck, MD
Jasvinder S. Bhatia, MD
Jean M. Francis, MD
Lauren D. Stern, MD
Pulmonary
John Bernardo, MD
Nicholas A. Bosch, MD
Christine L. Campbell-Reardon, MD
Finn J. Hawkins, MB, BCh
Elizabeth S. Klings, MD
Frederic F. Little, MD
George T. O'Connor, MD
Rheumatology
Andreea M. Bujor, MD, PhD
Monica P. Crespo-Bosque, MD
David T. Felson, MD, MPH
Eugene Y. Kissin, MD
Tuhina Neogi, MD, PhD
Michael R. York, MD
DEIA Week: Poster Submissions and Contribute to DEIA Week Celebration!
The Department of Medicine will hold its second annual Diversity, Equity, Inclusion and Accessibility (DEIA) Week March 10 - March 14, 2025. In the DoM, we are dedicated to fostering a workplace that values and celebrates diversity, promotes equity, ensures inclusion, and prioritizes accessibility. We firmly believe that our collective differences make us stronger, and we are committed to creating an environment where all individuals, regardless of their background, feel valued, respected, and empowered.
Monday, March 10th
Poster Showcase | Hiebert Lounge (Lunch will be served) | 11:30AM-1:30PM
Posters created by DoM faculty, staff, and trainees to illustrate the ongoing DEIA work in the areas of research, education, programming, patient care, and beyond.
Learn how to submit a poster to this year’s Poster Showcase here!!
Tuesday, March 11th
Panel + Discussion | Hiebert Lounge (Breakfast will be served) | 8AM-10AM
Wednesday, March 12th
Mindfulness Event | Location and time TBD
Thursday, March 13th
DEIA Week Celebration | Hiebert Lounge | 4:30PM-6:30PM
Contribute to the celebration here!
Friday, March 14th
Grand Rounds | Keefer Auditorium | 12:00PM-1:00PM
AY24 DoM Annual Report!