Sonia Ananthakrishnan, MD, Receives Stanley L. Robbins Award for Excellence in Teaching
Sonia Ananthakrishnan, MD, assistant professor of medicine, has been recognized with the Chobanian & Avedisian School of Medicine’s highest teaching honor, the Stanley L. Robbins Award for Excellence in Teaching.
The annual award honors an outstanding educator and acknowledges the importance of teaching skills and commitment to students and education. It was established in recognition of the exceptional teaching and devotion to students exemplified by Stanley L. Robbins, MD, former professor and chair of pathology.
“Dr. Ananthakrishnan achievements as a teacher, mentor, program developer, innovator, scholar and leader in medical education made her an outstanding candidate for this award,” a colleague said in recommending Ananthakrishnan for the award. “She identified the need to improve the quantity and quality of feedback and created a local and national reputation around the educational initiative of improving feedback exchanges across all levels of training in the department of medicine.”
Ananthakrishnan also found ways to improve the evaluation of medical student clinical reasoning skills. “As a clerkship director, she addressed the need for more high-quality assessment by creating the Observed Clinical Reasoning Assessments (OCRA). The OCRA has successfully integrated into the internal medicine clerkship and this style of examination has been adopted by several other clerkships (neurology and pediatrics) and even in the preclinical curriculum,” he added.
Ananthakrishnan has championed diversity, equity, inclusion and belonging on the medical campus. She is one of the original creators of the Lights On, Intent vs Impact, Full Stop, Teach (LIFT) training for bystanders, addressing micro-aggressions as part of the Mid-Career Faculty Leadership Program in 2020. The LIFT training program has been widely disseminated across the campus in part due to her work facilitating more than a dozen sessions for students, faculty and hospital leadership.
Ananthakrishnan has been active in medical student and resident education at the School since 2009. She has mentored hundreds of medical students as they travel through the residency application process consistently earning high praise including: “She is a role model for all educators having excelled in every educational domain including direct teaching, assessment, curriculum development and scholarship,” wrote the colleague in the letter of recommendation.
Ananthakrishnan currently serves as the Director of Student Education in the department of medicine and is the clerkship director to third-year students in the Medicine 1 clerkship. She has served as the faculty mentor for the Internal Medicine Interest Group at the School since 2012, the student-led group that plans activities designed to educate the student body on the field of Internal Medicine and its various subspecialties. She is an active national member of Clerkship Directors in Internal Medicine.
Ananthakrishnan’s outpatient practice is in endocrinology, diabetes and nutrition at Boston Medical Center with a focus in neuroendocrinology. She works as the endocrine director of a multidisciplinary neuroendocrine group and is a Spanish-speaking provider.
Finance Staff Development Sample Syllabus
Key Finance Concepts:
General Accounting
- Financial Statement Analysis
- Income Statements
- Understanding the Balance Sheet
Profit & Loss Statements
Budgeting
Financial Reporting & Analysis
Reporting
Excel
- Working with Data
- Creating Reports
- Advanced Excel formatting and formulas
Actual vs. Budget Variance
Department of Medicine Account Structure
Financial Modeling
Revenue/Cost Analysis
BU Research Administrator Resources
- BU Research Support
- Clinical Trial billing
- Effort Reporting - PAR
- Grant Management
- New Hire onboarding process
- Postdoc Onboarding
- BU Works
- BU Works training schedule
- If you don't see the training you'd like to attend, please email your request to ithelp@bu.edu.
- BU SAP training grid
- BU Works training schedule
- BU Works
- Procurement
Medical Grand Rounds – April 7
Medical Grand Rounds
Friday, April 7 | 12:00-1:00 PM | Keefer Auditorium (Hybrid)

Joseph Korn Memorial Lecture: "Dissecting the Complex Phenotype of Scleroderma Vasculopathy"
Presented by:
Tracy Frech, MD
Associate Professor of Medicine
Rheumatology & Immunology Division
Vanderbilt University
Medical Center
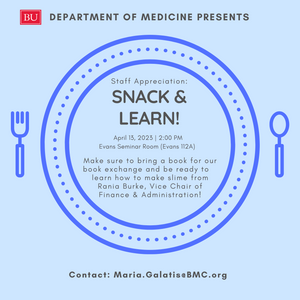
DoM Staff Appreciation: Snack & Learn
Join us for our monthly staff appreciation event! Bring a book for the book exchange and enjoy a snack and coffee with colleagues.
2023 Annual Faculty & Staff Awards Recipients
Honoring the outstanding service of faculty and staff members of Boston University Chobanian & Avedisian School of Medicine is an important aspect of our school, so it gives me great pleasure to announce these 2023 awards. Please join us in congratulating the recipients.
Educators of the Year
Preclerkship
Ricardo Cruz, MD, MPH
Assistant Professor of Medicine/General Internal Medicine
Stanley L. Robbins Award for Excellence in Teaching
Sonia Ananthakrishnan, MD
Assistant Professor of Medicine/Endocrinology, Diabetes & Nutrition
Leonard Tow Humanism in Medicine Award
Laura Wung, MD
Assistant Professor of Medicine/General Internal Medicine
Equity, Inclusion & Accessibility:
Faculty
Elizabeth Klings, MD
Professor of Medicine/Pulmonary, Allergy, Sleep & Critical Care Medicine
Medical Grand Rounds – March 24
Medical Grand Rounds
Friday, March 24 | 12:00-1:00 PM | Keefer Auditorium (Hybri d)
d)
Gary Garber Memorial Lecture: "From textile dyes to starch: Unraveling the mystery of cardiac amyloidosis"
Present by:
STARDoM – Employee Recognition Program
We are excited to announce the "STARDoM" Employee Recognition Program to acknowledge out standing non-faculty employees!

Medical Grand Rounds – Alan Farwell, MD
"Sick Euthyroid Syndrome: Is there anything new?"
Friday, March 10th | 12:00-1:00PM | Keefer Auditorium (Hybrid)

Presented by:
Zoom Meeting Information
https://bostonu.zoom.us/j/92577463257pwd=RWtXZDFlUGV6UjQxc2szYzZjQ0RSZz09
Meeting ID: 925 7746 3257
Passcode: 890982
FY24 Research Accelerator Program
The Department of Medicine Research Accelerator Program is to provide support for junior faculty who are committed to pursuing a career as a physician-scientist or scientist within the DOM. The program provides funding during the crucial period of career development in the first three years of their first faculty position (Instructor or Assistant Professor) within the DOM. Eligible MD or MD/PhD. applicants can be final year senior fellows or junior faculty members. Eligible PhD post-doctoral fellows must be in the final year of training with pending appointment to faculty independent of this award. This program does not support individuals to continue post-doctoral studies.
For more information click here.
Submit your applications as a single pdf by April 15, 2023 to Vanessa.Nguyen@bmc.org.