USOM II
Case 1: A 32 y/o M motorcyclist struck the side of a moving motor vehicle at high speed, was thrown 15 feet, and transiently lost consciousness per bystanders. Prehospital vital signs were as follows: P: 120, BP: 100/palpitation, SpO2: 95%, RR: 25, GCS 9/15. In the Emergency Department, the patient was A&Ox3 with a GCS of 15 and labored respirations. The patient reported left shoulder pain and shortness of breath. Initial ED vitals: HR 125, RR 25-30, SpO2 97% RA, blood pressure nonpalp by automated cuff, with no radial pulses and faint femoral pulses. The patient’s airway was intact and b/l breath sounds were present. Providers noted mild anterior chest tenderness without ecchymosis or deformity. A left shoulder joint dislocation was noted. US performed:
What ultrasound exam was performed above and what are the significant findings?
Answer
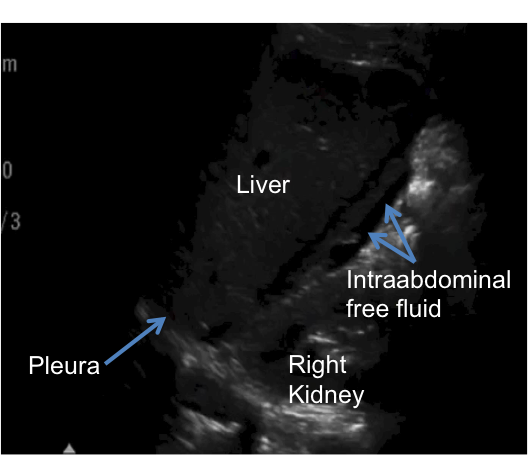
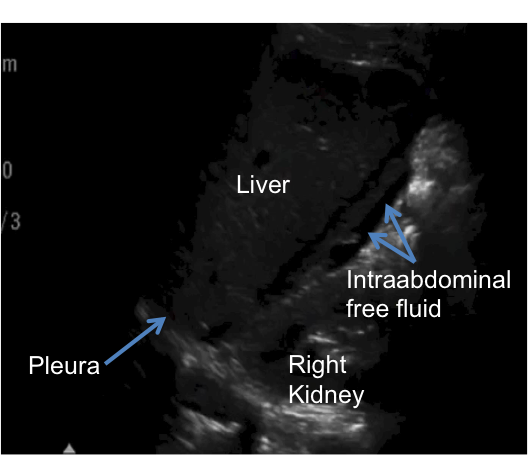
The video demonstrates an eFAST (Expanded Focused Assessment with Sonography in Trauma). This study incorporates both the abdominal FAST exam with a thoracic exam to evaluate for hemo- or pneumothorax. The FAST in this case reveals hypoechoic fluid in the RUQ view (Morrison’s Pouch), which is the most sensitive view in a FAST to identify intraperitoneal fluid (#1).
How effective is the FAST exam? What is the sensitivity and specificity?
Answer
The FAST is an integral component of a trauma evaluation and per ATLS protocol should be performed after the completion of the primary survey. The FAST has variable sensitivities for the detection of intraperitoneal fluid (63-100%), but excellent specificity (95-100%). Approximately ~500-600 cc of fluid is necessary to yield a positive exam (#2, #3).
In the setting of blunt trauma, a positive FAST should elicit high suspicion for intraperitoneal bleeding. If the FAST is negative, but the patient remains hypotensive or unstable, additional investigation is indicated (i.e. computed tomography or exploratory laparotomy).
Case 2: The same patient above presents to your trauma bay:
What is the finding on this EFAST? How effective is ultrasound in detecting this pathology?
Answer
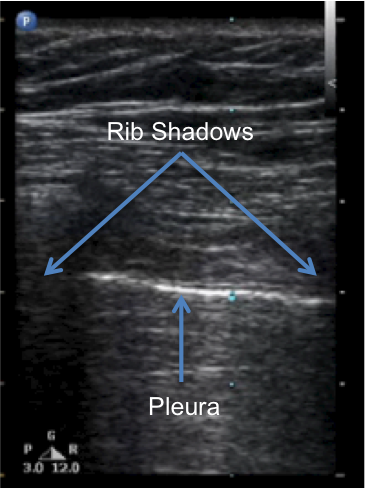
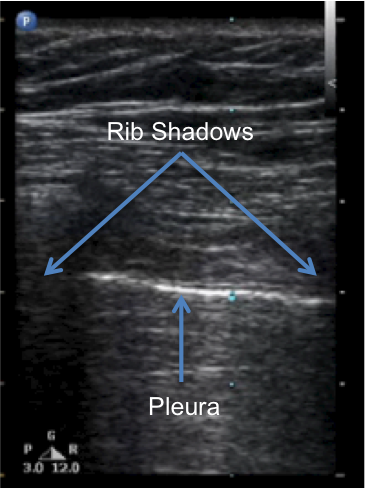
This patient has a pneumothorax. The hyperechoic linear line between the two rib shadows represents the pleura. In the previous case, one observes sliding between the visceral and parietal pleuras, a normal finding. The absence of lung sliding between pleural layers in this case reflects extrapulmonic air in the thorax, which is a pneumothorax. Ultrasound has a higher sensitivity than CXR in detecting pneumothorax (98.1% vs. 75.5%; #4).
Case 3: Same motorcycle patient presents and the following ultrasound is performed:
What condition is seen on this eFAST?
Answer
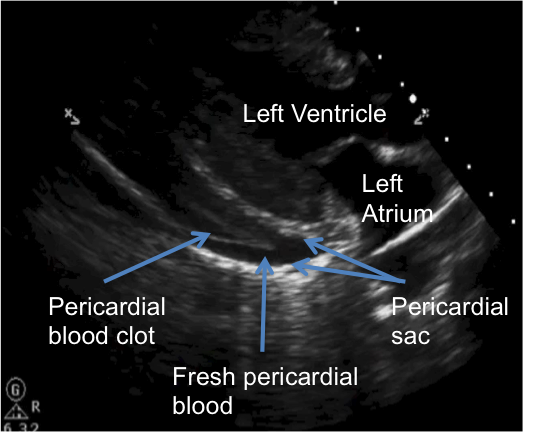
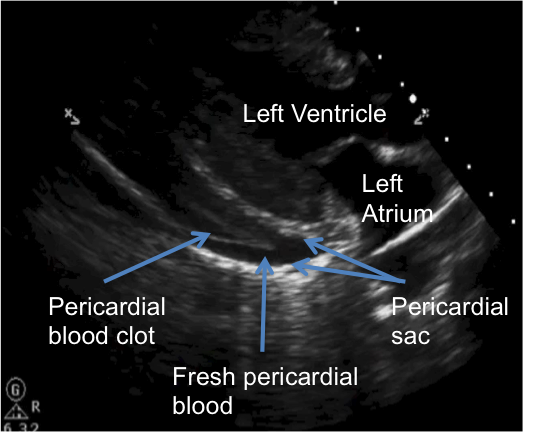
Pericardial effusion with evidence of both clot and fresh hemopericardium.
What’s the epidemiology and mechanism of this type of injury?
Answer
Hemopericardium in blunt trauma is relatively rare and is generally due to rupture of a free wall of the heart (right atrium 8-65%, right ventricle 17-32%, left atrium 8-15%, left ventricle 0-31%; #5). This injury carries a high mortality and only 5% of patients with blunt cardiac injury and hemodynamic instability survive to hospital admission (#6). This injury typically results from massive anterior thoracic forces, such as those in a motor vehicle collision. The injury mechanism often leads to a multi-system trauma in these patients and one may also observe other associated thoracic injuries such as sternal or rib fractures, pneumothorax, hemothorax, and pulmonary or cardiac contusions.
What is the sensitivity and specificity of transthoracic ultrasound in the detection of hemopericardium?
Answer
Sensitivity = 96% and specificity = 98% (#7).
What is the management of the patient above?
Answer
The patient presents with tamponade physiology and his injuries require immediate intervention. A stable patient with this injury should be taken directly to the OR for thoracotomy and definitive repair of the cardiac wall rupture. If the patient becomes hemodynamically unstable, then an ED thoracotomy may be considered. In patients with this injury who are hemodynamically stable (including low but stable blood pressure values), a pericardiocentesis may be considered. The drainage catheter would drain extra-cardiac volume and relieve the tamponade until more definitive care is possible.
What’s your airway management for this patient?
Answer
If the patient should manifest distress or deteriorating mental status, endotracheal intubation may be indicated. However, intubation could be dangerous for this patient, as positive intra-thoracic pressure (as occurs in mechanical ventilation) may severely reduce cardiac filling and lead to cardiovascular collapse. As such, intubation should ideally occur in the controlled environment of the operating suite.
References (back to top)
1) Rozycki, G.S.; Ochsner, M.G.; Feliciano, D.V.; et al. Early Detection of hemoperitoneum by ultrasound examination of the right upper quadrant: a multicenter study. J Trauma. 45(1998), pp. 878-883
2) Patel, Riherd. Focused assessment with sonography for trauma: methods, accuracy, and indications. Surg Clin N Am 91 (2011); 195-207.
3) http://www.uptodate.com/contents/emergency-ultrasound-in-adults-with-abdominal-and-thoracic-trauma
4) Blaivas, Ml Lyon, M; Sandeep, D. Prospective comparison of supine chest radiography an bedside ultrasound for the diagnosis of traumatic pneumothorax. Academic Emergency Medicine. Vol 12, Issue 9, Sep 2005; 844-849
5) Schultz, J.M.; Trunkey, D.D. Blunt Cardiac Injury. Crit Care Clin. 2004; 20(1):57-70
6) Fedaker, et al. Fatal traumatic heart wounds: Review of 160 autopsy cases. Isr Med Assoc J. 2005;7 498-501
7) Mandavia D.P.; Hoffner R.J.; Mahaney K.; Henderson S.O. Bedside echocardiography by Emergency Physicians. Ann Emerg Med. 2001;38(4):377