Medical Students with Blood Borne Pathogen Infections Policy
Policy on Medical Students with Blood Borne Pathogen Infections
Policy Statement
The Boston University Chobanian & Avedisian School of Medicine recognizes its duty to minimize the risk of transmission of blood-borne pathogens by individuals studying at the University, to maintain a supportive learning environment and to protect the patients that we serve. BUSM developed this policy to ensure that the school acts in a manner consistent with these duties.
Hepatitis B, Hepatitis C
Policy: Graduate medical, dental, and other health related students are considered Health care workers (HCW) as they enter the clinical arena. HCW recovering from Hepatitis B and Hepatitis C must be cleared by his/her own health care provider and Student Health Services prior to engaging in medical education activities including clinical training.
Work precautions: HCW with chronic Hepatitis B antigenemia must strictly observe infection control precautions and should refrain from practices and procedures where a risk of transmission exists as identified by the CDC and other public health authorities. Infection control precautions that apply to all HCW must be strictly observed, regardless of whether they perform invasive procedures:
(1) HCW should wear gloves for direct contact with mucous membranes or non-intact skin of all patients
(2) HCW who have exudative lesions or weeping dermatitis should refrain from direct patient care, having contact with the patient’s environment, handling patient equipment or devices used in performing invasive procedures until the condition resolves.
Mass. DPH Reportable Diseases, Surveillance, and Isolation and Quarantine Requirements
Human Immunodeficiency Virus Infection/AIDS
Policy: Individuals who are asymptomatic may continue to work in patient care areas. Every effort will be made to protect patients and other HCW from unnecessary exposure to infectious agents. As such, infected HCW must take precautions to prevent the transmission of blood or body fluids to patients or other HCW.
Clinical aspects: Acquired immune deficiency syndrome (AIDS) is caused by the Human Immunodeficiency virus (HIV). Transmission of this virus occurs through intimate or percutaneous/mucous membrane or open wound splash contact with infected blood or body fluids. A blood test is available for detection of viral load and antibody to HIV. A positive antibody to HIV may represent active infection, latent infection, or prior exposure to the virus.
Work precautions: HCW with HIV must strictly observe infection control precautions and should refrain from practices and procedures where a risk of transmission exists as identified by the CDC and other public health authorities. Infection control precautions that apply to all health care professions must be strictly observed, regardless of whether they perform invasive procedures:
(1) HCW should wear gloves for direct contact with mucous membranes or non-intact skin of all patients
(2) HCW who have exudative lesions or weeping dermatitis should refrain from direct patient care, having contact with the patient’s environment, handling patient equipment or devices used in performing invasive procedures until the condition resolves.
Mass. DPH Guide to Reporting, Surveillance and Control – Disease Chapter HIV
http://www.mass.gov/eohhs/docs/dph/disease-reporting/guide/hiv-aids.pdf, June 2006
Reason for Policy
The intent of this policy is to limit the possibility of transmission of blood-borne pathogens by infected students within both the educational and clinical setting, while maintaining a welcoming and non-biased learning environment.
Entities Affected By This Policy
- Medical Students
- Patients who have medical students involved in their care
- Faculty and administrators supervising the education of medical students
Scope
This policy applies to all medical students enrolled at BUSM, in the medical curriculum, including both BUSM and visiting medical students.
Procedure
General Considerations.
To decrease their risk of acquiring or transmitting blood-borne pathogens, all BUSM students involved in patient care receive training in the principles of Standard Precautions during the M1 and M3 orientation sessions. Students are expected to adhere to those principles at all times within all educational and clinical settings. Any student who believes that they may have exposed others to their blood or bodily fluids in a clinical situation has a professional responsibility to notify the attending physician or supervising faculty member and to comply with the applicable reporting and follow-up policies and protocols of the clinical site where the incident occurred. As professionals concerned with the health of others, it is strongly recommended that students involved in such incidents consent to undergoing diagnostic testing for blood-borne pathogens as defined below.
Students who are infected with a blood-borne pathogen must avoid circumstances in which they could potentially transmit their infection to others. It is therefore the professional responsibility of all students who are infected with blood-borne pathogens to self identify and report their infection status to Boston University’s Student Health Services at least 2 months prior to starting a clinical rotation.
BU SHS will notify Boston Medical Center’s Occupational Medicine Clinic (or other clinical training facility) 3 months before the start of a student’s clinical rotation so that appropriate procedures, if needed, may be adopted to minimize transmission risk to patients and team members. Any recommendations that substantially alter the student’s activities will be communicated to the Associate Dean of Student Affairs who will convene a meeting of the BUSM Technical Standards Committee to discuss any needed modifications in the educational program for the affected student, to ensure that the student will have a comparable curricular experience.
This policy is included in the policies that students are required to review at the beginning of each academic year. Students sign electronically attesting to this review.
Admission to the Medical School.
An applicant’s HBV, HCV, or HIV serologic status will have no impact on consideration for admission to BUSM.
Accommodations.
In compliance with the American with Disabilities Act Amendments Act of 2008 (ADAAA) students living with blood-borne diseases will not be discriminated against when considering admission and retention at BUSM.
Once it has been determined what if any adjustments or restrictions need to be imposed on an individual student, reasonable accommodations will be developed through the BU Disability Office and Technical Standards Committee. All BUSM students must meet the BUSM technical standards.
Appendices
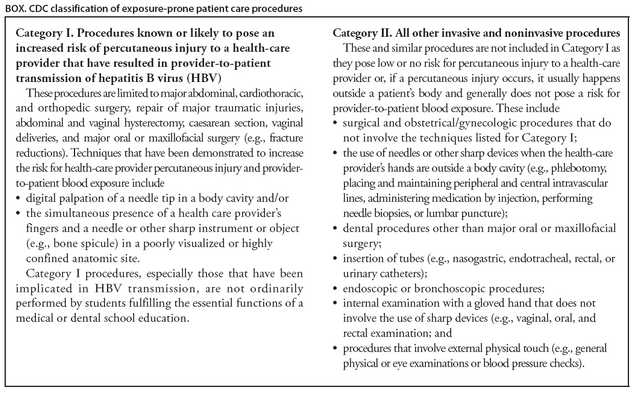
Appendix 1: Resources: current guidelines regarding exposure prone procedures for infected health care workers
From: Centers for Disease Control and Prevention; Updated CDC Recommendations for the Management of Hepatitis B Virus-Infected Health-Care Providers and Students; MMWR; 2012; 61: 3.
[Approved by the BUSM Executive Committee on January 15, 2019.]