Physicians Call for an End to Conversion Therapy
Conversion therapy is a broad term used to describe practices and actions aimed at changing people’s sexual orientation or gender identity – to turn anyone who doesn’t identify as “straight” into a “straight” person. Historically, conversion therapies have used electroshock therapy, chemical drugs, hormone administrations and even surgery. While these extreme practices are becoming rarer, many other harmful actions are still taking place, negatively impacting both children and adolescents as well as adults in the U.S., according to a perspective in this week’s New England Journal of Medicine.
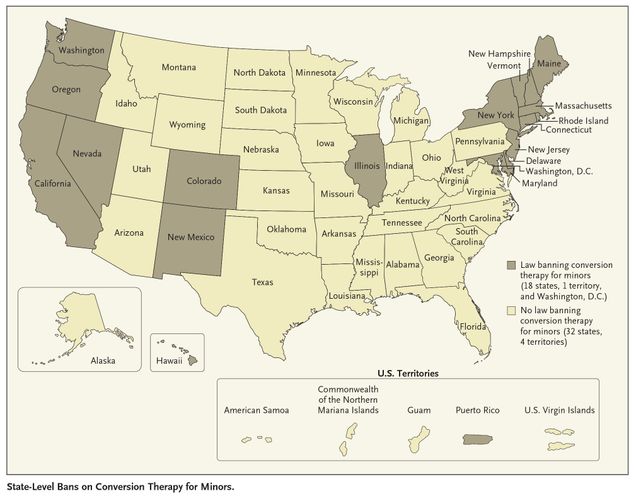 Graphic from New England Journal of Medicine perspective
Graphic from New England Journal of Medicine perspective
Currently, only 18 states have laws banning conversion therapy in the U.S. for people younger than 18 years old. No states have bans on conversion therapies done to adults. “As a result of the lack of regulation on these “therapies” many adults and children continue to be defrauded, harmed, and traumatized in the U.S. every day,” explains lead author Carl Streed, Jr., MD, MPH, FACP, assistant professor of medicine at Boston University School of Medicine and a primary care physician at Boston Medical Center (BMC).
According to the authors, the harm these therapies cause is well-documented, including higher rates of depression, suicidal thoughts and suicide attempts. “In addition to the health problems associated with conversion therapies, these practices also carry serious economic burdens for LGBTQ people and the country at large, including low educational achievement, lower income, and lower work performance,” said Dr. Streed, who also treats patients at the Center for Transgender Medicine & Surgery at BMC.
The perspective encourages physicians to be vigilant about this issue given that many victims of conversion therapy are often silent about it. The authors highlight the importance of teaching physicians about common traits and risk factors to help them better identify patients who underwent or may be undergoing conversion therapy. They also emphasize, for medical professionals, the psychiatric illnesses conversion therapies cause, such as post-traumatic stress disorder (PTSD) that require medical attention.
Of equal importance, they also call to action medical educators to reform the curricula of medical schools and training programs to better prepare future physicians to care for LGBTQ people, including identifying and treating past trauma. There is ample evidence that current physicians are ill-equipped to help victims of conversion therapy and LGBTQ people at large. This is largely because education on LGBTQ health is not a mandated part of medical schools’ curricula, and thus most doctors never learn to care for these patients general health needs properly-much less the trauma caused by conversion therapy.
“Put simply, these practices need to end,” said Dr. Streed. “We need to work across sectors to focus on ensuring that all individuals of all ages receive appropriate, comprehensive care by trained medical professionals in a supportive environment.”
Dr. Streed, who served as the former chair of the Massachusetts Medical Society Advisory Committee on LGBTQ Matters and the former chair of the American Medical Association Advisory Committee on LGBTQ Issues, advocates to end conversion therapy.
View all posts