Curriculum Overview
The BU Chobanian & Avedisian School of Medicine’s MD curriculum is an innovative four-year curriculum at the Frontlines of Medicine. Our instructional design principles and teaching methods incorporate best practices in learning theory, acknowledge the learning needs and styles of our diverse group of students and integrates science, health equity and clinical medicine. Our curriculum is designed to prepare our graduates for medical practice now and in the future.
The curricular goals of our MD program are to ensure that every BU Chobanian & Avedisian SOM graduate can:
- Establish and maintain medical knowledge necessary for the care of patients
- Demonstrate clinical skills and diagnostic reasoning needed for patient care
- Effectively communicate with patients, families, colleagues and interprofessional team members
- Practice relationship centered care to build therapeutic alliances with patients and caregivers
- Exhibit skills necessary for personal and professional development needed for the practice of medicine
- Demonstrate knowledge of health care delivery and systems needed to provide optimal care to patients and populations
- Exhibit commitment to promoting and advancing health equity for all patients
Curriculum Background
Our curriculum, redesigned in 2022, was created through a visioning process, that began and continued for five years before implementation, where medical school leaders, faculty, students and staff came together to describe the priorities of our MD program thinking about how healthcare will evolve in the future, the needs of the populations we serve and the many professional paths our students take after graduation.
The curriculum redesign process began with a review of the Carnegie Foundation report Educating Physicians: A Call for Reform of Medical School and Residency. Our curriculum now includes the principles described in the paper that called for (1) standardizing learning outcomes and individualizing the learning process, (2) promoting multiple forms of integration, (3) incorporating habits of inquiry and improvement, and (4) focusing on the progressive formation of the physician’s professional identity. Our instructional design is also based on learning theory and principles from Make It Stick: The Science of Successful Learning written by Roediger, McDaniel and Brown. Our curriculum focuses on interleaving, spaced learning and using multiple learning styles and strategies to promote long term retention and deep learning. We continuously evaluate and evolve our curriculum to ensure that our students are prepared to meet the needs of patients now and in the future. We also aim to help students explore their professional interests, identity and become leaders and scholars in medicine through explorations in the curriculum.
Curriculum Phases
The curriculum has three phases, the pre-clerkship phase, clerkship phase and post-clerkship phase. The goals and details of each phase are described below.
Pre-Clerkship Phase
The pre-clerkship phase objectives, content and instructional design are based on the following goals:
- Integration of foundational, clinical, social and health systems sciences in a systems-based curriculum
- Spaced Learning to Enhance Long Term Retention for Learners
- Promotion of Wellness and Professional Identity Formation of our Learners
- Educating students on how to promote and advance health equity for all patients
- Self-Regulated Learning and Developing Adaptive Expertise
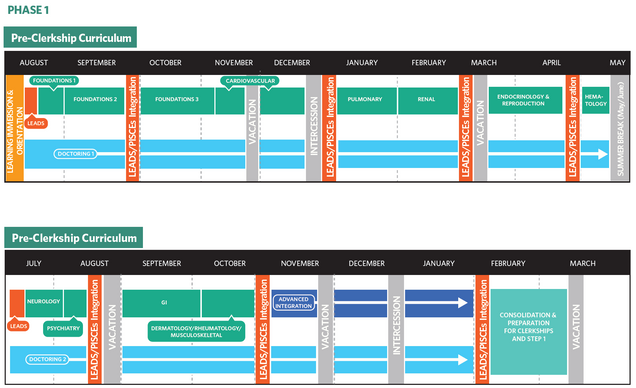
Students in the pre-clerkship phase of the curriculum are enrolled in four courses 1) Principles Integrating Science, Clinical Medicine and Equity (PISCEs), 2) Doctoring 3) Learn, Experience, Advocate, Discover and Serve (LEADS) and 4) Consolidation and Preparation for Clerkship.
Principles Integrating Science, Clinical Medicine and Equity (PISCEs)
PISCEs is a longitudinal integrated course that prepares students with the medical knowledge needed to care for patients. It integrates foundational science, pathophysiology and disease management. The course is broken into 3 foundational modules followed by eight systems-based (e.g., cardiovascular, neuro/psych) modules. Woven into each of these modules are longitudinal threads which include oncology, infectious disease, anatomy, microbiology, pharmacology and pathology, as well as the school’s health equity curricular themes.
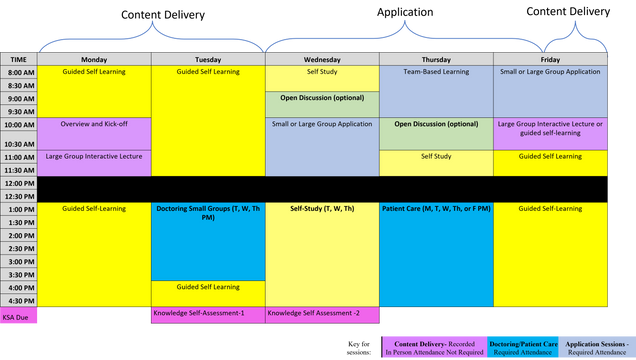
The PISCEs curriculum uses multiple instructional design strategies to support active learning, peer learning and team development. The instructional design of the course can be seen below:
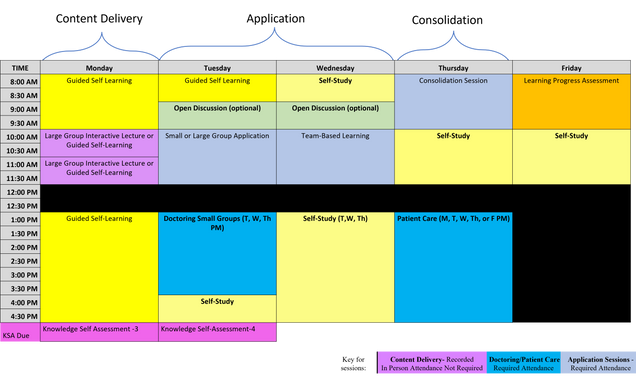
The last 10 weeks of the pre-clerkship curriculum, called the Advanced Integration Weeks, focuses on integrated cases based on the Core patient presentations organized by clinical areas and disciplines. Students will revisit prior foundational, clinical, and social science content in patient cases to help students consolidate and integrate the material. In these final ten weeks of the preclerkship phase, students are immersed each week in patient cases that begin with a patient presentation to a clinic or ER and then evolve over a week where students navigate patient signs, symptoms, labs and imaging to again connect foundational science to patient data they will see in clerkships. These cases also have a goal of introducing students to patient cases that are representative of our patient population at Boston Medical Center, our primary teaching hospital. All cases are based on real patient cases and integrate teaching about our unique populations highlighting knowledge and skills needed to address our curricular key themes and populations. Finally, students collaborate in small groups to solve clinical problems, simulating the “clinical team” in medical practice and review and prepare for the USMLE Step 1 exam.
Doctoring
Doctoring 1 is a year-long course in the first year where students learn foundational doctoring skills. The primary purpose of Doctoring 1 is to advance students’ skills in the ten doctoring domains (see below). Through the multiple components of the course, students will learn and practice medical interviewing, physical examination skills and clinical reasoning. They will explore relational competence in both direct patient care and in the small group role plays. Students will learn how to gather data during a medical encounter, including a structured approach to chronological history taking for the history of present illness and details of the additional components (ex. past medical history, past surgical history, family history, social history, allergies, medications, review of systems). Students will learn and practice physical examination techniques in small groups and in clinical encounters. These skills culminate in a systematic approach to the head-to-toe physical examination at the end of the second module.
As the course progresses and students enter their systems based PISCEs modules, students will build off their foundational physical exam skills to learn more advanced skills and physical diagnosis in the system they are learning about in their PISCEs course and this will continue into Doctoring 2. Students will develop the skills of communicating the components of the medical encounter in standard oral and written format. Additionally, oral presentation skills of research topics will be taught and evaluated in small groups. As the course progresses, clinical reasoning aka “how doctors think” will be utilized in evaluating symptom presentations. In all aspects of the course, health equity and disparities will be a lens students will use to reflect on their own backgrounds, on the lived experiences of their patients, and on their role as developing clinicians.

Doctoring 2 is a year-long course in the second year in which students build off their experience in Doctoring 1 enhancing their skills in the 10 doctoring domains. The course is structured in case-based small groups with a faculty member that allow practice of advanced communication and physical examination skills, as well as clinical reasoning skills. Some of the sessions will include actors or standardized patients to enhance the authenticity of the experiences. There will be a focus on hypothesis-driven data collection (i.e., asking history questions and performing physical examination maneuvers that increase or decrease the likelihood of the diseases on the differential diagnosis) and clinical reasoning. Students will refine and expand their case presentation and note-writing skills and be introduced to the electronic medical record. Cases will promote integration of foundational and social science topics and provide an opportunity for self-directed learning. Students will have a variety of additional simulation sessions and actor/standardized patient interviews to further their skills. They will continue their clinical placements with a longitudinal preceptor in the fall and will participate in hospital-based clinical encounters with 4th year medical student and faculty preceptors during the winter/spring to further advance their clinical skills in preparation for their clinical clerkships. Students will continue to work on their teamwork skills and competence in building a therapeutic alliance with patients and will reflect on topics surrounding professionalism, ethics, and professional identify formation.
Learn, Experience, Advocate, Discover and Serve (LEADS)
LEADS is a two-year course intended to provide our students with time in the formal curriculum to immerse themselves in learning, experience and discovery in health equity so that they can develop skills in designing scholarly innovations now and in their future careers.
The LEADS health equity curriculum begins with an overview of health equity and the inequities in health that exist due to factors at the personal, social, political, and other structural levels. The course has students consider the role physicians have in recognizing and addressing adverse social determinants of health and the inequities and injustices that contribute to health disparities. The health equity areas of focus in this course include: LGBTQIA+ Health, Global and Refugee Health, Community Health, Homeless Health, Structural Determinants of Health, Racism in Medicine, and Addiction and Health. All areas of focus have a faculty lead(s) who are content experts and deliver core knowledge in the course and provide mentorship and work with students to develop individualized goals.
The curriculum also engages students in experiential opportunities to advance their understanding of inequities and allow students to further witness the challenges marginalized patients face. Students are introduced to BMC faculty, staff, and community leaders who will share solutions and interventions that have led to improved health outcomes. Longitudinally students engage in regular journal clubs highlighting evidence-based interventions related to health equity and are taught scholarly methods to make change including research methods, educational methods, health systems science, community based and advocacy interventions.
Finally, students learn ways to disseminate their ideas including through narratives, curricula and other formats. Students are responsible for designing a scholarly project focused on a potential intervention of change in their health equity focus area by the completion of the course.
As part of this course, students can join a Longitudinal Research Track as part of the Medical Student Research Program and will be mentored in a 3- to 4-year experience designed for students who want to immerse themselves in research. Students in this track participate in additional required extracurricular hours with their research team outside of the LEADS curriculum.
Consolidation and Preparation for Clerkship
This course includes time for Step 1 preparation and study followed by a transitional clerkship in which students participate in experiences focused on understanding the learning environment of the clerkship year and the core skills needed throughout the clerkship phase.
The United States Medical Licensing Examination (USMLE) is a national, three step examination for medical licensure in the U.S. Students must take Step 1 and Step 2 CK during their time in the MD Program. For more information on state-specific licensing requirements, please see the State Authorization website.
Clerkship Phase
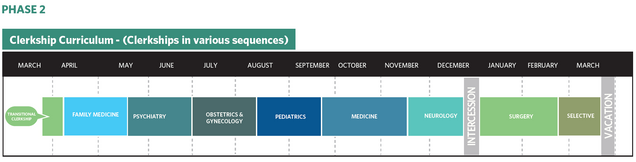
The core clerkship year follows the preclerkship phase. Students complete clinical clerkships in medicine, surgery, pediatrics, obstetrics/gynecology, family medicine, neurology, and psychiatry. Students work with residents and attending physicians in the care of a broad range of patients and clinical conditions. Students rotate through multiple clinical settings including ambulatory and inpatient and rural, urban and suburban, depending on their site placement ad preference. Students also have one selective of their choice in Emergency Medicine, Radiology or Research that they can choose during the third year.
The core clerkship year concludes with a week-long transition to 4th year experience that prepares students for the expectations of a sub-intern.
Post-Clerkship Phase
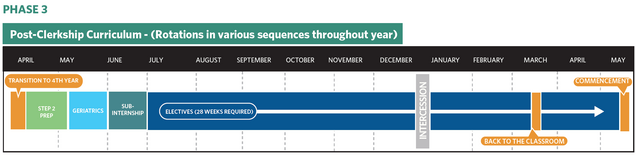
Upon completion of the core clerkship year, students complete advanced clinical rotations in geriatrics and home care, a sub-internship in the specialty of their choice and 6 months of electives. The third and fourth years combined include a minimum of 24 weeks of elective time with opportunities to pursue clinical and basic science research, teaching skills as well as independent study programs. Students also must complete a longitudinal requirement in Teaching, Advocacy, Research, Advocacy or Quality Improvement in their additional months of fourth year. Students may also participate in a specialty specific electives designed to prepare students for the transition to residency.
Students can view information about currently offered electives via the Fourth Year Course Catalog, available on the Registrar’s Website.
Visit Our Registrar’s Office
Registrar’s Office