Success of New Hyperglycemia Crisis Management Guideline
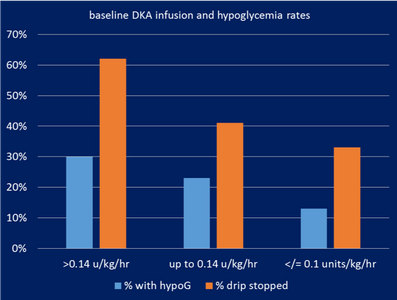
In AY2018 the Endocrine Subcommittee of the Pharmacy and Therapeutics Committee rolled out changes to the longstanding BMC Hyperglycemic Crisis Management Guideline, which had been in use for more than a decade. A QI project done the prior year had shown higher rates of hypoglycemia (blood glucose (BG) <70) in patients after up-titration of the insulin infusion drip, in particular to doses of >0.14 unit/kg/hour of insulin. These patients had a 3-fold higher rate of hypoglycemia, and in 60% of patients treated at this dose needed to have the drip stopped to prevent hypoglycemia (Figure 1).
Led by Dr. Sara Alexanian the Director of Inpatient Diabetes Program and Quality Leader in the Section of Endocrinology, a multidisciplinary group including en
docrine, pharmacy, nursing and IT came together to create an updated guideline. The process included reviewing primary literature supporting current hyperglycemic crisis management, review of national standards as well as protocols at outside institutions. Based on this review a new guideline was developed. Major changes included:
- Removal of default increases in the insulin infusion rate, and
- An updated insulin titration algorithm based on solid published evidence.
Subsequently there were several months of ED and ICU nursing education, including – in-services by endocrine and pharmacy, as well as a required Health Stream course. The new guideline was rolled out in September 2019.
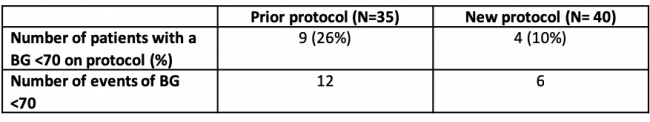
Three months after the release of the new guideline, a chart review was done on the 40 patients who were treated with the new algorithm compared to 35 patients on the prior protocol. There was a 60% reduction in hypoglycemia (26% on the prior protocol down to 10% on the new protocol, Table 1). Furthermore the total episodes of hypoglycemia decreased with the new protocol, as did the number of times the drip needed to be stopped to prevent hypoglycemia. Further analysis showed that despite the lower rates of hypoglycemia, there was no significant increase in the time to DKA resolution.
The multidisciplinary workgroup continues to engage with nursing to improve the guideline. Based on feedback, new changes include making minor adjustments to the insulin titration algorithm and making the transition to dextrose-containing fluids a default in the order set to ease nursing work-flow. Furthermore, when substantial discrepancies occur between the ED and ICU weights, the nurse will be prompted to adjust the infusion dose appropriately for weight obtained on admission to the ICU. These changes are expected to go live in the fall 2019 with the hope of reducing hypoglycemic events further!