News
- Students enjoyed attending the The 2019 Program Retreat, particularly they keynote address from alumnus Dr. Hao Ngyuen, MD PhD
- Aditya Mithal (G3) was awarded a travel award and abstract trainee merit award for his poster at the 2019 Annual Meeting of the International Society for Stem Cell Research.
- Omar Mohtar’s (M3) recent JCB publication has been highlighted as an editor’s choice in Science Signaling. Check it out here.
- Shen Ning (G3) has been featured in a Journal of NeuroPhysiology Podcast discussing her work investigating how sleep-wake cycles affect tau accumulation. This podcast can be found here.
- Congratulations to our six graduates in the Class of 2019!
- Nisma Mujahid (Class of 2019) was featured in a PBS Nova Article discussing sun protection, something that she investigated in her graduate studies. This article can be found here.
- Marc Vittoria, G4, NIH F30
- Nisma Mujahid, ’19, Canadian Institutes of Health Research Doctoral Foreign Study Award, Gold Humanism Honor Society
- Jacob Kantrowitz, ’19, Gold Humanism Honor Society
- Leon Sun, G4, NIH F30
- Alissa Frame, M3, NIH F31, Best Poster Award at American Heart Meeting on Hypertension
- Terry Hsieh, ’18, Alpha Omega Alpha, Travel Award from the Shock Society,Gold Humanism Honor Society
- Anjali Jacob, ’19, NIH F31, Jo Rae Wright Young Investigator of the Year, FASEB meeting – best trainee oral presentation, First Author Paper in Cell Stem Cell, Alpha Omega Alpha
- YoonJoo Lee, G4, NIH F30, Travel Award from American Society for Cell Biology
- Will Li, G4, Autism Science Foundation – Predoctoral Fellowship
- Sanghee Lim, M3, Medical Student Grants Targeting Melanoma and Skin Cancer Research,Melanoma Research Foundation Medical Student Research Grant
- Melody Lun, ’18, Society for Neuroscience Trainee Professional Development Award
- Ryan Quinton, G4, Canadian Institutes of Health Research Doctoral Foreign Study Award, Jean McPhail Award
- Stephanie Pavlovich’s M4 new Cell Paper can be found here
Congratulations to our MD-PhD Class of 2025 AOA Inductees!
We are proud and honored to announce the following AOA inductees from our MD-PhD Class of 2025.
Congrats to our 2025 graduates!
Congratulations to our 2025 MD-PhD graduates Eric Bressler, Sean Corcoran, Neelou Etesami, Keith Gagnon, Jarrod Moore, and Allison Tipton!
- Eric will begin residency in surgery and research in the Physician Scientist Training Program at Stanford University
- Sean will begin residency in Internal Medicine and research in the Physician Scientist Training Program at Cedar's Sinai Medical Center
- Neelou will begin residency in Internal Medicine at The University of California, Los Angeles
- Keith will begin residency in surgery and research in the Physician Scientist Training Program at The Ohio State University
- Jarrod will begin residency in Internal Medicine at The University of California, Los Angeles
- Allison will begin residency in psychology and research in the Physician Scientist Training Program at The University of North Carolina at Chapel Hill
We wish you all the best in your upcoming endeavors!
From left to right: Neelou Etesami, Sean Corcoran, Jarrod Moore, Keith Gagnon, Allison Tipton, Eric Bressler
Celebrating our graduating M4s and rising M3s!
Celebration is in full effect for our graduating M4s who all matched into their desired residencies and our rising M3s who all successfully defended their dissertations this spring! MD PhD students gathered together at Estragón to hear congratulatory remarks from Co-Directors Dr. Trinkaus-Randall and Dr. Borkan, and to celebrate with their peers. This annual event celebrates the accumulation of years of hard work. Congrats to each student! We wish our graduating M4s the best of luck as they get ready to embark on their new journey that is residency training. To our rising M3s, good luck and have fun during clinical rotations!
Graduating M4 Residency Placements:
University of California, Los Angeles - Internal Medicine
Ohio State University - General Surgery PSTP
Stanford University - General Surgery
University of North Carolina - Psychiatry PSTP
Cedar Sinai - Internal Medicine PSTP
Dissertations:
Andrew Chang - Volatile anesthetic induced patterns of disruption in neuronal communication within the C. Elegant nervous system
Anthony Spinella - Age-Associated Alterations in Head and Neck Cancer
Nathan Sanders - Animal Models of Coronavirus Heterotypic Immunity
Kelley Anderson - Molecular Subtypes of Airway Field Gene Expression Alterations are associated with Lung Cancer Phenotypes
Laura Garcia Marshall - Limbic Afferent and Intrinsic Innervation Patterns in the Primate Nucleus Accumbens Shell
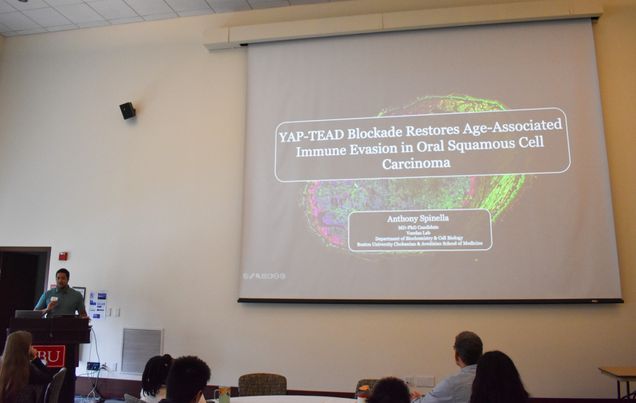
Congratulations to Anthony Spinella on a successful defense!


Congratulations to Anthony Spinella on successfully defending his PhD dissertation entitled Age-Associated Alterations in Head and Neck Cancer!
Anthony is a member of the Varelas Lab in BU's Department of Biochemistry & Cell Biology. In 2024, he was selected to present a research talk at the FASEB Hippo Pathway in Biology and Diseases Conference in Melbourne, FL, where he discussed his work on YAP-TEAD blockade and its role in restoring age-associated immune evasion in oral squamous cell carcinoma. He also presented a selected research talk at the 2024 Boston University School of Medicine MD-PhD Annual Retreat. Additionally, Spinella was awarded Best Poster Presentation at the Biochemistry & Cell Biology Department Annual Retreat at BUSM. In 2023, he gave a selected research talk at the American Physician Scientist Association Northeast Regional Meeting. In 2022, Spinella was honored with the Best Lightning Talk Award at the Genome Science Institute 2022 Research Symposium and also won Best Poster Presentation at the 2022 Biochemistry Department Annual Retreat at BUSM.
Anthony was awarded an F30 by the National Institute of Aging, focused on defining age-associated alterations in oral squamous cell carcinoma. Anthony was also awarded a Student Seed Grant by the Boston University Center for Multiscale and Translational Mechanobiology to explore the mechanical properties of the oral tumor microenvironment in aged tissues.
Congratulations again, Anthony, and we wish you all the best moving forward. 🎉
Abstract Summary:
Head and neck squamous cell carcinomas (HNSCC) are the seventh most common cancers globally with poor survival rates and largely ineffective pharmacological treatments. Despite older age being associated with worse survival for HNSCC, most preclinical cancer studies focus on outcomes in young animals, potentially contributing to the limited understanding and treatment strategies for these cancers. To test the influence of age on HNSCC, we utilized carcinogen-induced and syngeneic orthotopic isograft models of HNSCC, performing hemi-lingual injections of murine oral squamous cell carcinoma cells that phenocopy tobacco-driven HNSCC in young and old mice. Old animals exhibited more rapid tumor growth, reduced intra-tumoral immune infiltration, and were enriched for transcriptionally-distinct, immune-evasive tumor cell populations. We observed that older age promotes malignant features in oral lesions. Additionally, we identified an enrichment of an age-associated, immune-evasive carcinoma cell population that coincided with reduced immune infiltration in tumors in old mice, molecular features that corresponded to reduced immune infiltration in human HNSCC. We further identified an age-associated, pro-fibrotic fibroblast population in the aged oral microenvironment that corresponded to elevated collagen deposition and elevated yes-associated protein (YAP) and TEA-domain transcription factor family (TEAD) activity in oral carcinoma cells in old mice. We demonstrated that targeting YAP-TEAD activity restored the immunogenicity of oral carcinoma cells, enhancing immune infiltration and tumor clearance in old mice. In additional studies, we demonstrated that correcting absent chemokine signaling in old mice and could restore intra-tumoral immune infiltration to promote tumor clearance and that induction of an age-associated, fibrotic stroma in young mice could recapitulate both the growth dynamics and immune-evasive phenotypes in oral carcinoma cells observed in old mice. Overall, these studies highlight the critical importance that aging plays in directing tumor biology in HNSCC, that YAP-TEAD contribute to mediating these dynamics, and that targeting age-associated alterations in the carcinoma cell, immune, or stromal compartments could serve as viable avenues for therapeutic intervention to improve outcomes for older HNSCC patients.
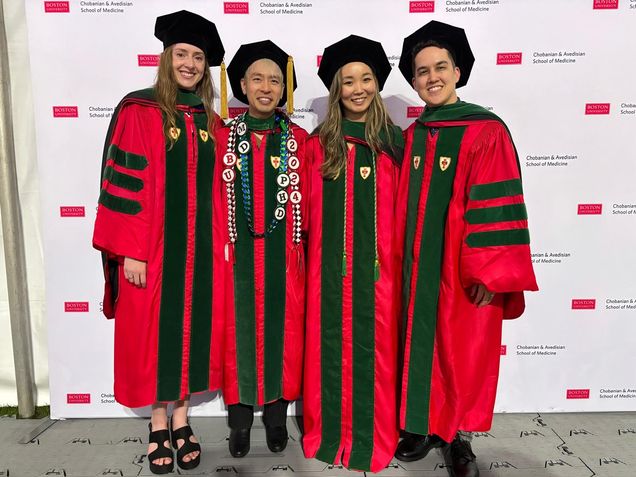
Congrats to our 2024 graduates!
Congratulations to our 2024 MD-PhD graduates Margaret Minnig, Anthony Yeung, Shen Ning, and David Swain!
- Margaret will begin residency in psychology and research at The University of Washington
- Anthony will begin residency in pediatrics as part of the Molecular Medicine Program at The University of California San Francisco
- Shen will begin residency in Diagnostic and Interventional Radiology at Massachusetts General Hospital
- David will begin residency in ophthalmology at Northwestern University
We wish you all the best in your upcoming endeavors!
Alumni Spotlight: Dr. Andre P. Cap MD PhD

Andre P. Cap, MD/PhD
BUCASM MD/PhD Class of 2003
Colonel, US Army (retired, November 2023)
Subject matter expert advisor to Joint Trauma System (JTS), US Pacific Command & US Special Operations Command (SOCOM)
Consultant: Velico Medical
Volunteer faculty member: Uniform Services University and Brook Army Medical Center
Borkan: How did your career unfold after BUSM?
Cap: My career took turns that I could not have predicted. It began as an M3 on the BMC Heme/Onc wards back in the day. we were giving a [chemotherapy] “martini” for CML…and they were dropping like flies... it was really a profound experience for me. Being 30 years old and wanting to do public service before I was “too old”, I substituted my MD/PhD fellowship for the Army for the last two years, did an Army residency in internal medicine and a hematology/oncology fellowship in Washington D.C. I thought I was going to be a bone marrow transplanter. But the Army asked, “Are we storing blood right and how can we make it more available in the battlefield?”. The DoD moved the Institute of Blood Research to San Antonio, Texas and they said, “You have PhD, why not take over the institute?” I became division director and then director of research for the whole institute right out of my fellowship. It was just pure luck…right place at the right time. I spent the next 15 years at the Army Institute of Surgical Research, mostly building and running the lab, and doing part-time clinical work at Brook Army Medical Center. So, I oversaw a $60 million per year research program and nearly 300 researchers. I did not intend to make it a 22-year career.
Borkan: What were your challenges?
Cap: In the beginning, it was “Whoa”. I was overwhelmed and there was skepticism. “You just finished fellowship, buddy”. I had to just sell my plans for the lab and myself as somebody who could execute those plans. It was wartime [in Iraq]. In the middle of a war, my superiors said, “Well, all right, let’s give this guy a try because what the hell, we’ve got to execute and execute now. So, let's see what he does”. I had trained in Joe Loscalzo’s lab, the former head of cardiovascular medicine, studying homocysteine and its effects on nitric oxide, bioavailability, and on endothelial function and platelets. Though it wasn't directly related, he gave his students independence, and it was self-driven research work...good for me to prepare for what lay ahead, even though I didn't know it at the time.
Borkan: What did you discover at the Institute to help our soldiers?
Cap: In the “old days”, people who were bleeding mostly received refrigerated (cold) whole blood, but people stopped doing that because of the fear that cold platelets wouldn't work. Well, it turns out they work just fine in whole blood, just like stored platelet concentrate…this observation led to the rebirth of whole blood, which is now all the rage in trauma management across the world. Instead of giving people emergency saline, we now give group O, low anti-A, anti-B titer whole blood as a universal product to improve oxygen delivery and hemostasis. Randomized DoD funded clinical trials show better outcomes with whole blood than components. I “backed into” the field of transfusion medicine from Heme-Onc and my fellowship training in bone marrow transplant.
Borkan: What motivated you to stay in research?
Cap: I did an elective during my PhD at the Brigham in vascular pathology. The medicine teams and surgery teams would present clinical cases in the “bowels of Brigham” where the pathologist showed autopsy specimens and labs like “very old school medicine”! The pathologist ran the meeting and you “touched the disease”, like aortic atherosclerosis...making what we did in the lab very real by handling the body. My PhD was actually in the department of Pathology. More than anything else, this motivated me to stick with research.
Borkan: How did BUSM training help your career?
Cap: I got a tremendous clinical training at BU that prepared me well for all the crazy things I enjoyed being in the army partly because it wasn't all just lab work. I deployed to Iraq… as chief of medicine of a combat unit at an Iraqi support hospital where I oversaw massive transfusion and really bad coagulopathies upfront in patients. I launched to Germany and worked in the ICU where I took care of many trauma patients. Now I get calls from all over the world about critically ill patients with hematologic problems or requests to help set up research programs. That's because of the synergy between the research and the clinical interest.
Borkan: What is your advice for our current MD/PhD students wondering how the use their dual degrees?
Cap: If you are open to trying to use both degrees and open to unusual opportunities that that might present, you can have a super interesting career. Accept a fair amount of uncertainty… it's hard to do both clinical medicine and research but not impossible. We can be the triple threats as a great administrators, clinical leaders and researchers but not all at the same time… When I joined the Army, people thought I had lost my mind. “You’re not doing anything interesting”. I think it was pretty interesting. There are also tremendous opportunities using your tools to work in the clinic and in the lab. I said to myself “I'm going to do this now” and this created opportunities along the way that capitalize on “what is great”. That's my advice.
Program Alumnus Dr. Aly Elezaby is Keynote Speaker at Annual MD-PhD Retreat!

Photo courtesy of Brittny Garcia
Annual MD-PhD Program Retreat Brings Students of All Years Together for a Day Full of Science, Medicine, Mentorship, and Fun!
The annual retreat is a student-planned initiative attended by all members of the MD/PhD training program. Students interact and learn from their colleagues in all years during this event. The retreat includes a keynote speaker (usually an alum of the program), several student scientific and clinical presentations, and a poster session where M2s and all students in the graduate phase of the program present research from their labs or rotations.
This year's alumni speaker is Dr. Aly Elezaby. Dr. Elezaby is an advanced heart failure and transplant cardiology at Stanford University School of Medicine and a research scientist in the lab of Dr. Daria Mochly-Rosen. He graduated from the MD-PhD program at Boston University School of Medicine in 2017.
Photos courtesy of Brittny Garcia
Congratulations to Daniel Kirsch on a successful defense!

Congratulations to Daniel Kirsch on successfully defending his PhD dissertation on the pathological contributions to clinical symptoms of CTE!
MD PhD Students Shine at Medical Student Research Symposium!

MD PhD students presented this past Monday at the Medical Student Research Symposium. Rose Zhao was selected as an oral presenter for her research on "Characterization of Whole-genome Double Sequencing Events Across Tissues in vivo." Martin Ma and Kristen Segars both won awards for their poster presentations. A huge congratulations to our students!