News
- Students enjoyed attending the The 2019 Program Retreat, particularly they keynote address from alumnus Dr. Hao Ngyuen, MD PhD
- Aditya Mithal (G3) was awarded a travel award and abstract trainee merit award for his poster at the 2019 Annual Meeting of the International Society for Stem Cell Research.
- Omar Mohtar’s (M3) recent JCB publication has been highlighted as an editor’s choice in Science Signaling. Check it out here.
- Shen Ning (G3) has been featured in a Journal of NeuroPhysiology Podcast discussing her work investigating how sleep-wake cycles affect tau accumulation. This podcast can be found here.
- Congratulations to our six graduates in the Class of 2019!
- Nisma Mujahid (Class of 2019) was featured in a PBS Nova Article discussing sun protection, something that she investigated in her graduate studies. This article can be found here.
- Marc Vittoria, G4, NIH F30
- Nisma Mujahid, ’19, Canadian Institutes of Health Research Doctoral Foreign Study Award, Gold Humanism Honor Society
- Jacob Kantrowitz, ’19, Gold Humanism Honor Society
- Leon Sun, G4, NIH F30
- Alissa Frame, M3, NIH F31, Best Poster Award at American Heart Meeting on Hypertension
- Terry Hsieh, ’18, Alpha Omega Alpha, Travel Award from the Shock Society,Gold Humanism Honor Society
- Anjali Jacob, ’19, NIH F31, Jo Rae Wright Young Investigator of the Year, FASEB meeting – best trainee oral presentation, First Author Paper in Cell Stem Cell, Alpha Omega Alpha
- YoonJoo Lee, G4, NIH F30, Travel Award from American Society for Cell Biology
- Will Li, G4, Autism Science Foundation – Predoctoral Fellowship
- Sanghee Lim, M3, Medical Student Grants Targeting Melanoma and Skin Cancer Research,Melanoma Research Foundation Medical Student Research Grant
- Melody Lun, ’18, Society for Neuroscience Trainee Professional Development Award
- Ryan Quinton, G4, Canadian Institutes of Health Research Doctoral Foreign Study Award, Jean McPhail Award
- Stephanie Pavlovich’s M4 new Cell Paper can be found here
MD PhD Students Shine at Medical Student Research Symposium!

MD PhD students presented this past Monday at the Medical Student Research Symposium. Rose Zhao was selected as an oral presenter for her research on "Characterization of Whole-genome Double Sequencing Events Across Tissues in vivo." Martin Ma and Kristen Segars both won awards for their poster presentations. A huge congratulations to our students!
Alumni Spotlight Interview: Milissa Kaufman MD PhD

Dr. Milissa Kaufman is a graduate of the combined MD/PhD program at Boston University. Dr. Kaufman is the medical director at the Hill Center, a clinical program specializing in the treatment of trauma-related disorders.
SCB: Describe your journey to BUSM?
MK: Honestly, I thought entering BUSM from Arizona State as an undergraduate was an unachievable dream. I nearly flunked out of high school. Then I went to a community college, where I struggled with undiagnosed learning disabilities. I was not someone who was prime for academia or medical school…but I had this burning interest from an early age to understand people's minds… I started to read about psychiatry, and I knew that was what I wanted to do. But I wondered, “How am I ever getting into medical school?” I did not know any doctors. I had to take fewer classes at a time than most students because it was harder for me to study. But I worked very hard, switched my degree from a BA to BS ( I could not learn a foreign language), and entered the Honors college. There, I had to write a thesis. A friend suggested his mentor, a Reproductive Biologist as my PI, so I worked in her lab and even stayed there for a few years after college. The lab became family to me. I loved the environment…that we were all working together, focused on a Quest. We published my thesis, which was a gigantic thrill to me. It was then I finally realized I maybe could become a doctor. But I did not go to medical school for 3 years. I was nervous to take the MCAT, but my PI continuously encouraged me. My first score was not great, and I did not get accepted. So, I took an MCAT course and increased my score just enough. I had not yet said my dream aloud to anybody…I wanted to study psychological trauma and dissociation and become a psychiatrist. Without thinking I had much of a chance, I decided to pay the $75 fee and apply to BU. Boston was where many of the trauma researchers whose work I had read worked. The day I day I got accepted to BU was one I will never forget! Such a thrill! I entered the MD program and was asked to join the MD/PhD program my second year. I struggled with anatomy…the Dean met with me and casually said, “Oh, this happens every year”…So, they sent me for testing, and this confirmed that I had a learning disability. Now I finally understood why school has always been so challenging! One part of my disability is “visual spatial,” which explained why I could not do gross anatomy. But this realization changed my life.
SCB: After medical school, how did you transition to your PhD years?
MK: I ended up doing behavioral neuroscience for my PhD studies. I was truly fortunate to be accepted at the National Center for PTSD to do my dissertation research, located the Boston VA Hospital, headed by Terry Keane. Dr. Keane is an expert is psychological trauma and one of my heroes. I remember nervously walking into his office for the first time. I let him know I was interested in PTSD, and I had read all his work. I also told him that what I really want to study was trauma-related dissociation. He told me: “Do you really want to study dissociation and ruin your career?” However, he almost immediately told me he would support my goal, “as long as you do good science, the field needs it!” Dr. Keane was so wonderful. I was his first MD/PhD student, and he was excited about that, too. I spent five and a half years in graduate school working with pioneers in the trauma field. They threw me right into ongoing clinical studies and I learned about psychiatric diagnostic assessment, interviewing, and psychometrics. This experience set me up for success in a later psychiatry residency. The most important part of my training at VA was working with combat veterans who had PTSD. From them, I learned how to identify traumatic dissociation. Some vets were “doubly traumatized” with childhood abuse and combat-related PTSD. Many of them were dissociative and that was what I wanted to understand. As an aside, but an important part of my story: A bonus part of my training was that the atmosphere at the VA was very accepting. I came out in graduate school. I came out as gay. It seemed like it was an okay thing to do…That was a gift that I did not expect, to be okay in my skin for the first time.
SCB: How did you find your psychiatry residency…and how did they find you?
MK: The MGH/McLean Psychiatry Training Program was another career dream! It was a terrific training environment. The faculty is devoted to supporting residents. Plus, McLean Hospital was only one of maybe 2 or 3 units in the country that had specialty programs for women with PTSD and dissociative identity disorder (DID). My passion really was to study and treat the dissociative subtype of PTSD and DID, and at MGH/McLean, I found like-minded people. It was a long journey from being a college kid in Phoenix, Arizona who could barely get through high school to MGH/McLean! During residency, I worked with trauma experts including Dr. Sherry Winternitz, who ran the clinical trauma programs. She was highly supportive when I told her I wanted do a neuroimaging study to understand the brain basis of traumatic dissociation in DID. Despite there only being one project on dissociation ever supported by NIH, she was determined to help me. Dr. Winternitz facilitated seed funding for my lab through a significant philanthropic donation. This donation was from a family who care deeply about child abuse survivors.
SCB: What jump started your independent research into trauma and dissociation?
MK: It seemed like synchronicity! Following residency training, I became the medical director of a treatment program for women with PTSD and DID. There, I began recruiting patients for our first study exploring the brain basis of traumatic dissociation. Then, as luck would have it, soon after, trauma expert Kerry Ressler, MD/PhD came to McLean and became the chief scientific officer. He arrived with a generous spirit, and he paid for my brilliant Post-Doc, Lauren Lebois, PhD. My little lab - which at the time was doing only a single neuroimaging study – suddenly grew. I had my ideas about the brain basis of dissociation and, thankfully, Dr. Lebois could really write! Within months, she received an F32 training grant. We then started working with an NIH program officer who was open to studying dissociation in traumatized individuals…soon after we got an R21. This was the project that I have been fantasizing since I was in college --- identifying biomarkers for traumatic dissociation. We began publishing our findings and then received RO1 funding. Many had said to me, “You'll never get NIH funding to study traumatic dissociation.” But it was my passion, and I also had so many mentors along the way who were saying, “Do what you want to do!” That is my story. I now have a research program. The dual degree program at BU started this whole career for me. BU believed in me. It really has been a dream come true.
SCB: How did BUSM help your career goals?
MK: I had wonderful experiences everywhere I trained. But there was something special about BU and the Mission. BUSM draws a particular type of person, and the faculty at BU always had this passion, this Mission to serve. Important to me, they were not driven by ego but by the Mission itself. BU felt like home to me…there were always ups and downs, yet the faculty made it seem like it was okay. It was okay to be a little different and to go your own way. Some of my colleagues who also had challenges along the way turned out to be some of the most accomplished students. The faculty were so proud of them! BU training emphasizes doing things...it is a “doer’s program.” And many of my colleagues had dreams like me and went on to do exactly what they had dreamed possible. I am so glad to be able to finally say, “Thank you. BU.” Being at BU changed my life in in so many ways…it changes who you are as a person.
11/24/2023
Interviewer: Dr. S. Borkan
Nobel Prize for Medicine Goes to BU MD PhD Alum!

We congratulate Drew Weisman MD/PhD (class of 1987) in receiving the Nobel Prize in Physiology or Medicine! The Nobel Prize in Physiology or Medicine was awarded to Drew Weissman and Katalin Karikó for their breakthrough discoveries in mRNA technology that led to COVID vaccines.
Photo by Peggy Peterson/Courtesy of Penn Medicine.
Congratulations to Shen Ning on her AOA Induction!

Shen Ning has been elected to have membership to the medical honor society, Alpha Omega Alpha (AOA). Induction into AOA is awarded to medical students who exemplify scholarship, character and have contributed significantly to the medical sciences and practice. On behalf of Boston University Chobanian & Avedisian School of Medicine's MD/PhD program, we would like to extend our warmest congratulations to Shen!
Shen now joins the ranks of the following MD/PhD students:
2022:Aditya Mithal, Kristy Abo, Katelyn Trecartin
2020: Ryan Quinton
2019: Marek Kowalski, Chris Gromisch and Iris Trutzer
2018: Anjali Jacobs
Congrats to our 2023 graduates!
Congratulations to our 2023 MD/PhD graduates Kristy Abo, Katelyn Batterman, Alissa Frame, Xu Ke, Yoonjoo Lee, Will Li, Jane Lock, Aditya Mithal, and Marc Vittoria! We wish you the best in your upcoming endeavors!
Read the Fall 2022 Bench to Bedpost Bulletin Here!
 The Fall 2022 edition of the Boston University MD/PhD Bench to Bedpost Bulletin is now live! Some highlights from this semester's Alumni edition include:
The Fall 2022 edition of the Boston University MD/PhD Bench to Bedpost Bulletin is now live! Some highlights from this semester's Alumni edition include:
- Dr. Borkan's interview with Dr. Ian Francis (MD/PhD '20)
- A recap of the 2022 annual MD/PhD Retreat
- Two award-winning MD/PhD students
- And more!
The Bench to Bedpost Bulletin is brought to you by Aria Pearlman Morales, Morgan Corniquel and Katie Hohl, all chairs of the Alumni Committee Branch of the MD/PhD Student Government.
Conor Shea wins Moorman-Simon Fellowship
Congratulations to Conor for winning the 2022-2023 Moorman-Simon Fellowship! The fellowship is provided to current MD/PhD and PhD students in Computational Biomedicine who are working in the field of cancer research. Conor has been working in Beane and Spira-Lenburg Labs, using single cell RNA transcriptomics to profile premalignant lesions in the lungs and identify their progression to cancer.
Learn more about the fellowship here.
New paper from David Swain: Investigating the morphological changes induced by glaucoma
Congratulations to David Swain for his new paper studying endothelial glycocalyx morphology in primate eyes with induced glaucoma published in Cells this month! The work provides another puzzle piece in our ongoing investigation into the pathophysiology of glaucoma, mainly the effects of decreased outflow on the trabecular outflow pathway. Read more about his work here.
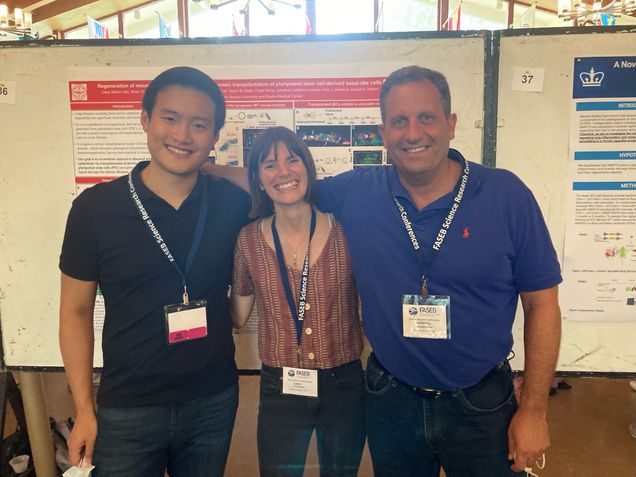
Congratulations to Martin Ma for winning a poster prize at the FASEB Lung meeting
Congratulations to Martin Ma from Darrell Kotton's lab for winning a poster prize at the FASEB Lung meeting! Martin’s poster was about using iPSC derived epithelial cells for airway regeneration.
Here is a picture of Martin at the poster presentation with his PI and fellow MDPhD classmate Carly Merritt!
Alumni Spotlight Spring 2022 – Dr. Ian Francis
Dr. Ian Francis is 2020 graduate of our program who is now a resident at Baylor College of Medicine’s Pediatrician-Scientist Program, located in Houston, Texas. He met with Dr. Borkan to discuss his experiences both in and out of our training program, and what he has learned along the way.
"What are the most valuable aspects of your dual degree, training?"
I considered this a broad question, looking back from at my time at BU, through what i'm doing now at Baylor College of Medicine and Texas Childrens Hospital. To me, both degrees share a perfect core element, an integration of two worlds: clinical science and the scientific understanding and I was drawn to both-from the first moment that I began Introduction Problems (IP) at BU. In class, we would go completely off road to and turn these basic, first year med student case presentations into questions we might ask in the lab. I really loved this learning approach of medicine and science just mashed together. At Texas Childrens, we spend half of half of our rounds talking about “What questions does the patient in Room 3 make you consider?” I enjoy a path that is more than just trying to get through each 10-hour shift. I enjoy thinking with both sides of my brain every day: the clinician side and the research side of your brain. It's so valuable that I'm trying to explicitly build it in our curriculum for residents, probably the first such program in the country, but certainly our institution’s first pediatric scientist training curriculum.
"What problems need to be solved in your chosen field of expertise?"
“Clinically, I'm pursuing pediatric intensive care, which is part of the reason I'm drawn to the space where so many clinical problems need to be solved. Surprisingly, even to this day, clinical inquiry into the clinical care of kids has not exactly been taboo, but is taken with an extreme level of caution. Children are a very sensitive population; they are at risk and are “delicate”. Partly as a result, there is a frustrating lack of data and science to guide the decisions that we make with our patients, especially in our intensive care unit. We often extrapolate from adult data and basic physiology to make clinical decisions even in the era of evidence-based medicine. There are so many scientific questions to be asked, especially in my worlds of microbiology and immunology acquired during my PhD training at BU. A question that firmly lives firmly in my brain, at intersection of these two scientific worlds, is why, why does the same infection have different outcomes in the NICU? Currently, we do not have accurate predictors (without rhyme or reason) for why clinical courses are so different for our septic kids. I'm really interested in the interplay between the immune system and the micro-invaders that tip some kids over the edge into immune dysregulation and septic organ failure. I hope that inquiry can define some of the pre-sepsis immune programs and microbial virulence factors needed to improve our targeted therapies. I would start with pseudomonas infections, which have a huge burden of disease that could truly impact the lives and health of the children I see.
“What advice would you share with our current md PhD students?”
For all levels MD/PhD training is such a remarkably unique path to walk because day by day, your “hat” is changing. What served me the best was walking into even the most unlikely of circumstances with an open mind, a willingness to be surprised, and also excited by anything and everything in front of me. Looking back at my time at BUSM, I was so sure that I would do vaccine development… these early experiences helped me to become the scientist I am. But afterwards, as I encountered new researchers, new labs, and new people, I was shocked at what else there was around me that opened my mind. Opening up my mind to other clinical problems to be solved in the ICU setting has excited me, and I’m running with it.
“What important lessons, did you learn during the transition between your dual degree, training and career path?”
Continuing to challenge both sides of the MD/PhD mind during your clinical time during residency that is so all encompassing and demanding. Even if we're lucky enough to be in a physician scientist training program, it is difficult to take productive steps during the final admission of the day. It is challenging to ask: “What does this patient offer me from a scientific standpoint? What question can I ask for it, even if it’s not profound: “Why am I using this medication for this patient?” or “Why is this the “standard?”. “For this presentation, what does this lab actually tell me about what's going on in my neutropenic patient?”. Even stopping to think “Why am I rechecking a CBC again, only hours later” will make me a better clinician. It helps to practice asking “why”, in order to keep my curiosity strong. We never know which one of our questions will balloon into a bigger question and a larger pursuit. Everyone's dream as a physician scientist is to find that question, then go back to the lab to chase it down.
“What attracted you to the research track during your residency training?”
Ian Francis: The research tracked placed both respect and emphasis placed on both science and medicine. This track included monthly meetings for just our pediatric scientists program residents to attend a journal club, career talk or network research progress to explore a dual path, which is hard and is not pre-paved. This is a rocky hike up the side of a mountain and there's no shame in and finding those things that help inspire this journey. When this track fits, others are here to throw me a rope to find my way…particularly to shield me when I need protected research time…this is a luxury and I see it as invaluable for my continued research training.
Contact: ian.francis@bcm.edu
Final words: “If it speaks to your heart, we truly need pediatric research scientists. You will find welcoming arms, unlike any other specialty."







