Alumni News
Have an update you want to share with our community? Email us at mdphdalu@bu.edu
Alumni Spotlight: Dr. Andre P. Cap MD PhD

Andre P. Cap, MD/PhD
BUCASM MD/PhD Class of 2003
Colonel, US Army (retired, November 2023)
Subject matter expert advisor to Joint Trauma System (JTS), US Pacific Command & US Special Operations Command (SOCOM)
Consultant: Velico Medical
Volunteer faculty member: Uniform Services University and Brook Army Medical Center
Borkan: How did your career unfold after BUSM?
Cap: My career took turns that I could not have predicted. It began as an M3 on the BMC Heme/Onc wards back in the day. we were giving a [chemotherapy] “martini” for CML…and they were dropping like flies... it was really a profound experience for me. Being 30 years old and wanting to do public service before I was “too old”, I substituted my MD/PhD fellowship for the Army for the last two years, did an Army residency in internal medicine and a hematology/oncology fellowship in Washington D.C. I thought I was going to be a bone marrow transplanter. But the Army asked, “Are we storing blood right and how can we make it more available in the battlefield?”. The DoD moved the Institute of Blood Research to San Antonio, Texas and they said, “You have PhD, why not take over the institute?” I became division director and then director of research for the whole institute right out of my fellowship. It was just pure luck…right place at the right time. I spent the next 15 years at the Army Institute of Surgical Research, mostly building and running the lab, and doing part-time clinical work at Brook Army Medical Center. So, I oversaw a $60 million per year research program and nearly 300 researchers. I did not intend to make it a 22-year career.
Borkan: What were your challenges?
Cap: In the beginning, it was “Whoa”. I was overwhelmed and there was skepticism. “You just finished fellowship, buddy”. I had to just sell my plans for the lab and myself as somebody who could execute those plans. It was wartime [in Iraq]. In the middle of a war, my superiors said, “Well, all right, let’s give this guy a try because what the hell, we’ve got to execute and execute now. So, let's see what he does”. I had trained in Joe Loscalzo’s lab, the former head of cardiovascular medicine, studying homocysteine and its effects on nitric oxide, bioavailability, and on endothelial function and platelets. Though it wasn't directly related, he gave his students independence, and it was self-driven research work...good for me to prepare for what lay ahead, even though I didn't know it at the time.
Borkan: What did you discover at the Institute to help our soldiers?
Cap: In the “old days”, people who were bleeding mostly received refrigerated (cold) whole blood, but people stopped doing that because of the fear that cold platelets wouldn't work. Well, it turns out they work just fine in whole blood, just like stored platelet concentrate…this observation led to the rebirth of whole blood, which is now all the rage in trauma management across the world. Instead of giving people emergency saline, we now give group O, low anti-A, anti-B titer whole blood as a universal product to improve oxygen delivery and hemostasis. Randomized DoD funded clinical trials show better outcomes with whole blood than components. I “backed into” the field of transfusion medicine from Heme-Onc and my fellowship training in bone marrow transplant.
Borkan: What motivated you to stay in research?
Cap: I did an elective during my PhD at the Brigham in vascular pathology. The medicine teams and surgery teams would present clinical cases in the “bowels of Brigham” where the pathologist showed autopsy specimens and labs like “very old school medicine”! The pathologist ran the meeting and you “touched the disease”, like aortic atherosclerosis...making what we did in the lab very real by handling the body. My PhD was actually in the department of Pathology. More than anything else, this motivated me to stick with research.
Borkan: How did BUSM training help your career?
Cap: I got a tremendous clinical training at BU that prepared me well for all the crazy things I enjoyed being in the army partly because it wasn't all just lab work. I deployed to Iraq… as chief of medicine of a combat unit at an Iraqi support hospital where I oversaw massive transfusion and really bad coagulopathies upfront in patients. I launched to Germany and worked in the ICU where I took care of many trauma patients. Now I get calls from all over the world about critically ill patients with hematologic problems or requests to help set up research programs. That's because of the synergy between the research and the clinical interest.
Borkan: What is your advice for our current MD/PhD students wondering how the use their dual degrees?
Cap: If you are open to trying to use both degrees and open to unusual opportunities that that might present, you can have a super interesting career. Accept a fair amount of uncertainty… it's hard to do both clinical medicine and research but not impossible. We can be the triple threats as a great administrators, clinical leaders and researchers but not all at the same time… When I joined the Army, people thought I had lost my mind. “You’re not doing anything interesting”. I think it was pretty interesting. There are also tremendous opportunities using your tools to work in the clinic and in the lab. I said to myself “I'm going to do this now” and this created opportunities along the way that capitalize on “what is great”. That's my advice.
Program Alumnus Dr. Aly Elezaby is Keynote Speaker at Annual MD-PhD Retreat!

Photo courtesy of Brittny Garcia
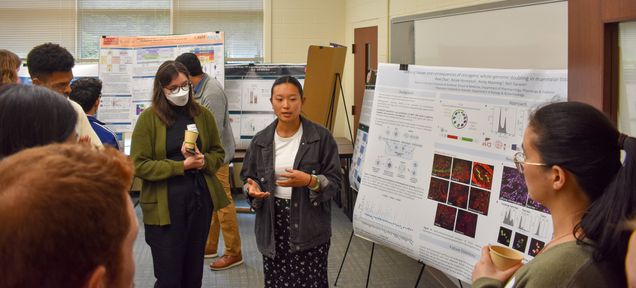
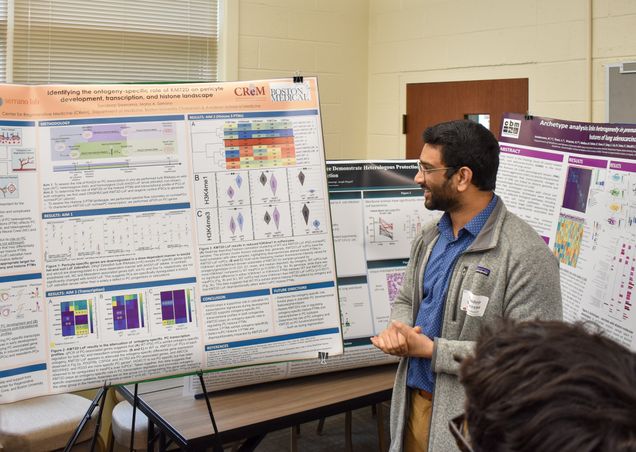
Annual MD-PhD Program Retreat Brings Students of All Years Together for a Day Full of Science, Medicine, Mentorship, and Fun!
The annual retreat is a student-planned initiative attended by all members of the MD/PhD training program. Students interact and learn from their colleagues in all years during this event. The retreat includes a keynote speaker (usually an alum of the program), several student scientific and clinical presentations, and a poster session where M2s and all students in the graduate phase of the program present research from their labs or rotations.
This year's alumni speaker is Dr. Aly Elezaby. Dr. Elezaby is an advanced heart failure and transplant cardiology at Stanford University School of Medicine and a research scientist in the lab of Dr. Daria Mochly-Rosen. He graduated from the MD-PhD program at Boston University School of Medicine in 2017.
Photos courtesy of Brittny Garcia
Alumni Spotlight Interview: Milissa Kaufman MD PhD

Dr. Milissa Kaufman is a graduate of the combined MD/PhD program at Boston University. Dr. Kaufman is the medical director at the Hill Center, a clinical program specializing in the treatment of trauma-related disorders.
SCB: Describe your journey to BUSM?
MK: Honestly, I thought entering BUSM from Arizona State as an undergraduate was an unachievable dream. I nearly flunked out of high school. Then I went to a community college, where I struggled with undiagnosed learning disabilities. I was not someone who was prime for academia or medical school…but I had this burning interest from an early age to understand people's minds… I started to read about psychiatry, and I knew that was what I wanted to do. But I wondered, “How am I ever getting into medical school?” I did not know any doctors. I had to take fewer classes at a time than most students because it was harder for me to study. But I worked very hard, switched my degree from a BA to BS ( I could not learn a foreign language), and entered the Honors college. There, I had to write a thesis. A friend suggested his mentor, a Reproductive Biologist as my PI, so I worked in her lab and even stayed there for a few years after college. The lab became family to me. I loved the environment…that we were all working together, focused on a Quest. We published my thesis, which was a gigantic thrill to me. It was then I finally realized I maybe could become a doctor. But I did not go to medical school for 3 years. I was nervous to take the MCAT, but my PI continuously encouraged me. My first score was not great, and I did not get accepted. So, I took an MCAT course and increased my score just enough. I had not yet said my dream aloud to anybody…I wanted to study psychological trauma and dissociation and become a psychiatrist. Without thinking I had much of a chance, I decided to pay the $75 fee and apply to BU. Boston was where many of the trauma researchers whose work I had read worked. The day I day I got accepted to BU was one I will never forget! Such a thrill! I entered the MD program and was asked to join the MD/PhD program my second year. I struggled with anatomy…the Dean met with me and casually said, “Oh, this happens every year”…So, they sent me for testing, and this confirmed that I had a learning disability. Now I finally understood why school has always been so challenging! One part of my disability is “visual spatial,” which explained why I could not do gross anatomy. But this realization changed my life.
SCB: After medical school, how did you transition to your PhD years?
MK: I ended up doing behavioral neuroscience for my PhD studies. I was truly fortunate to be accepted at the National Center for PTSD to do my dissertation research, located the Boston VA Hospital, headed by Terry Keane. Dr. Keane is an expert is psychological trauma and one of my heroes. I remember nervously walking into his office for the first time. I let him know I was interested in PTSD, and I had read all his work. I also told him that what I really want to study was trauma-related dissociation. He told me: “Do you really want to study dissociation and ruin your career?” However, he almost immediately told me he would support my goal, “as long as you do good science, the field needs it!” Dr. Keane was so wonderful. I was his first MD/PhD student, and he was excited about that, too. I spent five and a half years in graduate school working with pioneers in the trauma field. They threw me right into ongoing clinical studies and I learned about psychiatric diagnostic assessment, interviewing, and psychometrics. This experience set me up for success in a later psychiatry residency. The most important part of my training at VA was working with combat veterans who had PTSD. From them, I learned how to identify traumatic dissociation. Some vets were “doubly traumatized” with childhood abuse and combat-related PTSD. Many of them were dissociative and that was what I wanted to understand. As an aside, but an important part of my story: A bonus part of my training was that the atmosphere at the VA was very accepting. I came out in graduate school. I came out as gay. It seemed like it was an okay thing to do…That was a gift that I did not expect, to be okay in my skin for the first time.
SCB: How did you find your psychiatry residency…and how did they find you?
MK: The MGH/McLean Psychiatry Training Program was another career dream! It was a terrific training environment. The faculty is devoted to supporting residents. Plus, McLean Hospital was only one of maybe 2 or 3 units in the country that had specialty programs for women with PTSD and dissociative identity disorder (DID). My passion really was to study and treat the dissociative subtype of PTSD and DID, and at MGH/McLean, I found like-minded people. It was a long journey from being a college kid in Phoenix, Arizona who could barely get through high school to MGH/McLean! During residency, I worked with trauma experts including Dr. Sherry Winternitz, who ran the clinical trauma programs. She was highly supportive when I told her I wanted do a neuroimaging study to understand the brain basis of traumatic dissociation in DID. Despite there only being one project on dissociation ever supported by NIH, she was determined to help me. Dr. Winternitz facilitated seed funding for my lab through a significant philanthropic donation. This donation was from a family who care deeply about child abuse survivors.
SCB: What jump started your independent research into trauma and dissociation?
MK: It seemed like synchronicity! Following residency training, I became the medical director of a treatment program for women with PTSD and DID. There, I began recruiting patients for our first study exploring the brain basis of traumatic dissociation. Then, as luck would have it, soon after, trauma expert Kerry Ressler, MD/PhD came to McLean and became the chief scientific officer. He arrived with a generous spirit, and he paid for my brilliant Post-Doc, Lauren Lebois, PhD. My little lab - which at the time was doing only a single neuroimaging study – suddenly grew. I had my ideas about the brain basis of dissociation and, thankfully, Dr. Lebois could really write! Within months, she received an F32 training grant. We then started working with an NIH program officer who was open to studying dissociation in traumatized individuals…soon after we got an R21. This was the project that I have been fantasizing since I was in college --- identifying biomarkers for traumatic dissociation. We began publishing our findings and then received RO1 funding. Many had said to me, “You'll never get NIH funding to study traumatic dissociation.” But it was my passion, and I also had so many mentors along the way who were saying, “Do what you want to do!” That is my story. I now have a research program. The dual degree program at BU started this whole career for me. BU believed in me. It really has been a dream come true.
SCB: How did BUSM help your career goals?
MK: I had wonderful experiences everywhere I trained. But there was something special about BU and the Mission. BUSM draws a particular type of person, and the faculty at BU always had this passion, this Mission to serve. Important to me, they were not driven by ego but by the Mission itself. BU felt like home to me…there were always ups and downs, yet the faculty made it seem like it was okay. It was okay to be a little different and to go your own way. Some of my colleagues who also had challenges along the way turned out to be some of the most accomplished students. The faculty were so proud of them! BU training emphasizes doing things...it is a “doer’s program.” And many of my colleagues had dreams like me and went on to do exactly what they had dreamed possible. I am so glad to be able to finally say, “Thank you. BU.” Being at BU changed my life in in so many ways…it changes who you are as a person.
11/24/2023
Interviewer: Dr. S. Borkan
Nobel Prize for Medicine Goes to BU MD PhD Alum!

We congratulate Drew Weisman MD/PhD (class of 1987) in receiving the Nobel Prize in Physiology or Medicine! The Nobel Prize in Physiology or Medicine was awarded to Drew Weissman and Katalin Karikó for their breakthrough discoveries in mRNA technology that led to COVID vaccines.
Photo by Peggy Peterson/Courtesy of Penn Medicine.
Read the Fall 2022 Bench to Bedpost Bulletin Here!
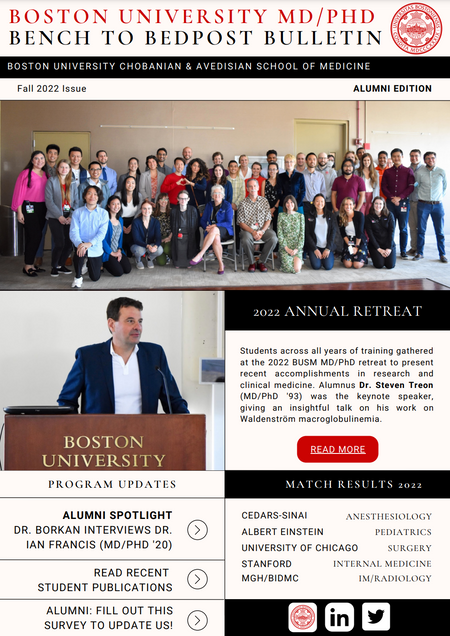 The Fall 2022 edition of the Boston University MD/PhD Bench to Bedpost Bulletin is now live! Some highlights from this semester's Alumni edition include:
The Fall 2022 edition of the Boston University MD/PhD Bench to Bedpost Bulletin is now live! Some highlights from this semester's Alumni edition include:
- Dr. Borkan's interview with Dr. Ian Francis (MD/PhD '20)
- A recap of the 2022 annual MD/PhD Retreat
- Two award-winning MD/PhD students
- And more!
The Bench to Bedpost Bulletin is brought to you by Aria Pearlman Morales, Morgan Corniquel and Katie Hohl, all chairs of the Alumni Committee Branch of the MD/PhD Student Government.
Alumni Spotlight Spring 2022 – Dr. Ian Francis
Dr. Ian Francis is 2020 graduate of our program who is now a resident at Baylor College of Medicine’s Pediatrician-Scientist Program, located in Houston, Texas. He met with Dr. Borkan to discuss his experiences both in and out of our training program, and what he has learned along the way.
"What are the most valuable aspects of your dual degree, training?"
I considered this a broad question, looking back from at my time at BU, through what i'm doing now at Baylor College of Medicine and Texas Childrens Hospital. To me, both degrees share a perfect core element, an integration of two worlds: clinical science and the scientific understanding and I was drawn to both-from the first moment that I began Introduction Problems (IP) at BU. In class, we would go completely off road to and turn these basic, first year med student case presentations into questions we might ask in the lab. I really loved this learning approach of medicine and science just mashed together. At Texas Childrens, we spend half of half of our rounds talking about “What questions does the patient in Room 3 make you consider?” I enjoy a path that is more than just trying to get through each 10-hour shift. I enjoy thinking with both sides of my brain every day: the clinician side and the research side of your brain. It's so valuable that I'm trying to explicitly build it in our curriculum for residents, probably the first such program in the country, but certainly our institution’s first pediatric scientist training curriculum.
"What problems need to be solved in your chosen field of expertise?"
“Clinically, I'm pursuing pediatric intensive care, which is part of the reason I'm drawn to the space where so many clinical problems need to be solved. Surprisingly, even to this day, clinical inquiry into the clinical care of kids has not exactly been taboo, but is taken with an extreme level of caution. Children are a very sensitive population; they are at risk and are “delicate”. Partly as a result, there is a frustrating lack of data and science to guide the decisions that we make with our patients, especially in our intensive care unit. We often extrapolate from adult data and basic physiology to make clinical decisions even in the era of evidence-based medicine. There are so many scientific questions to be asked, especially in my worlds of microbiology and immunology acquired during my PhD training at BU. A question that firmly lives firmly in my brain, at intersection of these two scientific worlds, is why, why does the same infection have different outcomes in the NICU? Currently, we do not have accurate predictors (without rhyme or reason) for why clinical courses are so different for our septic kids. I'm really interested in the interplay between the immune system and the micro-invaders that tip some kids over the edge into immune dysregulation and septic organ failure. I hope that inquiry can define some of the pre-sepsis immune programs and microbial virulence factors needed to improve our targeted therapies. I would start with pseudomonas infections, which have a huge burden of disease that could truly impact the lives and health of the children I see.
“What advice would you share with our current md PhD students?”
For all levels MD/PhD training is such a remarkably unique path to walk because day by day, your “hat” is changing. What served me the best was walking into even the most unlikely of circumstances with an open mind, a willingness to be surprised, and also excited by anything and everything in front of me. Looking back at my time at BUSM, I was so sure that I would do vaccine development… these early experiences helped me to become the scientist I am. But afterwards, as I encountered new researchers, new labs, and new people, I was shocked at what else there was around me that opened my mind. Opening up my mind to other clinical problems to be solved in the ICU setting has excited me, and I’m running with it.
“What important lessons, did you learn during the transition between your dual degree, training and career path?”
Continuing to challenge both sides of the MD/PhD mind during your clinical time during residency that is so all encompassing and demanding. Even if we're lucky enough to be in a physician scientist training program, it is difficult to take productive steps during the final admission of the day. It is challenging to ask: “What does this patient offer me from a scientific standpoint? What question can I ask for it, even if it’s not profound: “Why am I using this medication for this patient?” or “Why is this the “standard?”. “For this presentation, what does this lab actually tell me about what's going on in my neutropenic patient?”. Even stopping to think “Why am I rechecking a CBC again, only hours later” will make me a better clinician. It helps to practice asking “why”, in order to keep my curiosity strong. We never know which one of our questions will balloon into a bigger question and a larger pursuit. Everyone's dream as a physician scientist is to find that question, then go back to the lab to chase it down.
“What attracted you to the research track during your residency training?”
Ian Francis: The research tracked placed both respect and emphasis placed on both science and medicine. This track included monthly meetings for just our pediatric scientists program residents to attend a journal club, career talk or network research progress to explore a dual path, which is hard and is not pre-paved. This is a rocky hike up the side of a mountain and there's no shame in and finding those things that help inspire this journey. When this track fits, others are here to throw me a rope to find my way…particularly to shield me when I need protected research time…this is a luxury and I see it as invaluable for my continued research training.
Contact: ian.francis@bcm.edu
Final words: “If it speaks to your heart, we truly need pediatric research scientists. You will find welcoming arms, unlike any other specialty."
Alumni Spotlight – Fall 2021 – Anjali Jacobs

- What is your favorite BUSM experience or memory?
My MD/PhD training was definitely quite a journey. One of the happiest days of my life was the day when everything finally came together with my project…the day of my thesis defense. I was able to share with all the people who have helped me along the way...from the medical school to graduate school staff to the MD/PhD program directors, family and friends…even the Facility Cores. I had gotten so much help from so many people and the defense was the single day that I could personally thank everyone. It was a culmination of everything I have done…and a result of collaboration with all those I met. Even though some days were negative, I left my training with many positive memories.
- What are the most valuable aspects of your dual degree training?
There are several benefits of doing a PhD and then going back into medicine. One is the becoming curious about the issues that we’re facing in caring for patients…and many are missing answers. PhD training helped me to ask questions that generate conversation, making my residency training a lot more interesting and fun. The second is that our PhD trains us to give oral presentations...and tell a story. Story telling occurs every time I present a patient in front of others, pulling it together in allotted time, while sustaining listener’s interest. The third PhD benefit was the opportunity to interact with senior faculty, breaking down the usual hierarchy to share interesting ideas. Instead of being afraid to ask questions during my residency, I took an active role in my learning, just like during my PhD training.
- What attracted you to the research track during your residency training?
I wasn’t like super sure that I wanted to join pulmonary critical care when I entered pulmonary research as a doctoral student at BUSM. But I found pulmonary questions engaging, I fit in with pulmonary folks, and also realized that there’s interesting questions still to be answered. At the end of the day, I like helping people who are having trouble breathing. I now realize that there are several “research tracts”. Many residencies offer a “research pathway” but without a promised fellowship position thereafter. While this would have exposed me to like-minded researchers, it is challenging to actually do research during residency training and I do not suggest it. In my research tract training, I could have chosen to train in another specialty [other than pulmonary critical care], since physician-scientists are valued in many subspecialty fields. When I interviewed for residency, I also interviewed for my fellowship and was offered both...a big relief! In exchange for doing 2 years of residency training, I promised to do an additional year of research during my fellowship…a fair trade off since I want to be physician-scientist as my career and loved the pulmonary fellowship at UCSF. I would remind trainees that it is also possible to ask about fellowships during residency interviews and make contacts for the future…even if you choose residency and ultimately fellowship training at two different institutions. Admission into competitive fellowship programs can be harder and more complex due to their smaller size, so a guaranteed fellowship position is more valuable than I initially realized. While “short tracking” at one institution is not for everyone, I am so very, very grateful for this opportunity.
- What problem(s) need to be solved in your chosen field of expertise?
Although ARDS was unusual, it has become common in the SARS CoV2 era. During my PhD, I had been thinking about the lung injury, repair, and fibrosis. Other than mechanical ventilation and oxygen, we have little to offer for treating ARDS and many patients die. Some survivors appear in my pulmonary clinic with post-COVID lung diseases that is not yet understood. Now we have an explosion of questions to be answered in pulmonary critical care. I think about these questions because I see outcomes affecting human beings…it is definitely tragic to see patients dying and also feels inspiring. This crisis will happen again at some point in our lifetime...but maybe we will have a better idea of how help our ARDS patients.
- What additional training would have been valuable before you left BUSM?
I actually think our medical and research training was excellent. I do wish for training in stress management techniques. Residency was really hard (granted there was a global pandemic) but I did not previously consider mental health and activities outside of work that I enjoyed… as result, I found it really hard to attain a sense of life balance during residency. Residency support, including a therapist, made a huge difference in my happiness. I do think that it is one of the most important things I learned after leaving BUSM!
Contact info: anjali.jacob@ucsf.edu
Congratulations to our rising M3s on defending!
We are so proud of our students who are beginning their transition back into their clinical training. Below are our students and the titles of their thesis.
- Shen Ning (GPN, PI: Shelley Russek)- “Developing Targeted Magnetic Nanoparticles for Therapeutic Antibody Delivery in Alzheimer’s Disease”

- Margaret Minnig (GPN, PI: Valentina Sabino)- “The Role of Corticostriatal Pituitary Adenylate Cyclase Activating Polypeptide (PACAP) in Excessive Alcohol Drinking”
- Anthony Yeung (MTM, PI: George Murphy)- “Hematopoiesis in the Lung: From Development to Adulthood”


Congratulations to Geoffrey Ginsburg, MD/PhD ‘84 !
Join us in congratulating Geoffrey Ginsburg, MD/PhD ‘84 for being selected by the NIH All of Us Research Program to serve as next chief medical and scientific officer! We're excited to follow all of your exciting new work