Researchers Identify Previously Uncharacterized Gene Necessary for DNA Repair
Cells are constantly subjected to DNA damage from a range of internal and environmental sources. It is estimated that cells can experience as many as 100,000 DNA lesions per day. One of the most deleterious types of DNA lesions is the DNA double-strand break (DSB). Just one unrepaired DNA DSB may be enough to cause mutations or cell death leading to a wide range of pathologies including cancer, immune deficiency, premature aging and neurodegeneration.
To respond to the array of DNA lesions that occur, cells have developed a complex and coordinated series of steps involving DNA damage recognition, cell cycle arrest and signaling-induced activation of the DNA repair machinery – processes collectively referred to as the DNA damage response (DDR). In recent years, progress has been made in understanding how this process is initiated, however the later stages of this process, including long range DNA end-resection, is not well understood.
 A researcher from the Clarke Laboratory at Boston University retrieves samples from ultra-cold storage in liquid nitrogen.
A researcher from the Clarke Laboratory at Boston University retrieves samples from ultra-cold storage in liquid nitrogen.In a new study, researchers from Boston University Chobanian & Avedisian School of Medicine, Massachusetts General Hospital (MGH) and Harvard Medical School, identified several uncharacterized chromatin factors (proteins that regulate gene expression) that are recruited to sites of DNA damage, including the gene ZNF280A. Importantly, this gene is hemizygously deleted – meaning one of the two copies of alleles is missing—in a subset of patients with a human developmental syndrome called 22q11.2 distal deletion syndrome.
Interestingly, the gene that encodes for the ZNF280A protein resides on chromosome 22 at the 22q11.2 locus, the same genetic locus that is lost in a subset of 22q11.2 distal deletion syndrome patients. Patients who lose the specific locus where the ZNF280A gene resides have relatively severe clinical features including, microcephaly (abnormally small head), short stature and growth defects, global developmental delay, cognitive impairment and an improperly functioning immune system (immune deficiency).
All of these clinical features are common in other human disorders caused by mutations or deletions in known DNA repair genes. “Based on our discovery that ZNF280A is an important new DNA repair protein, we were interested to understand whether these patients were experiencing DNA repair defects and genomic instability in their cells, as a direct result of less ZNF280A expression, and wondered if this might explain some of their clinical features,” explains co-corresponding author Raul Mostoslavsky, MD, PhD, Scientific Director of the Krantz Family Center for Cancer Research at Massachusetts General Hospital and professor of medicine at Harvard Medical School.
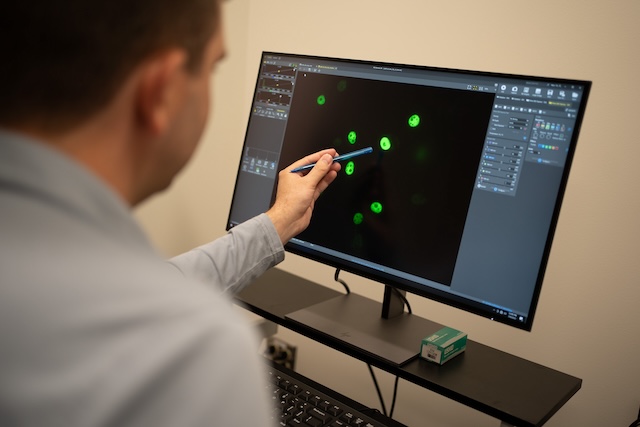 Thomas L. Clarke, PhD, assistant professor of Pathology, analyzing immunofluorescent microscopy images of human cells.
Thomas L. Clarke, PhD, assistant professor of Pathology, analyzing immunofluorescent microscopy images of human cells. “To date, identification of chromatin factors in DNA repair has been limited due to the lack of high-throughput screening methodologies. Moreover, traditional siRNA screens and more recent CRISPR knockout screening approaches have proved challenging in the context of chromatin factors, due to their essentiality for cell viability. Our current study provides strong evidence that our approach exploiting DNA open reading frame (ORF) sequences in a high throughput context has the potential to identify uncharacterized chromatin factors essential for DNA repair that may have been missed via conventional screening approaches,” explained co-corresponding author Thomas L. Clarke, PhD, assistant professor of pathology and laboratory medicine at BU.
The researchers used an innovative DNA repair screening approach developed in the Mostoslavsky lab specifically designed to identify chromatin factors that are recruited to sites of DNA damage. Using several distinct but complementary DNA repair assays, they confirmed that ZNF280A is important for repairing a DNA DSB.
The researchers then initiated a collaboration with clinicians at the Children’s Hospital of Philadelphia, who are leading experts in 22q11.2 distal deletion syndrome. As a result, they were able to use cell lines derived directly from patients with this syndrome with the specific deletion in the genomic locus where the ZNF280A gene resides (22q11.2; LCR22D-LCR22E). These cells have increased DNA damage and are defective in repairing DNA double-strand breaks. Notably, they were able to reintroduce ZNF280A into these cells which partially rescued these DNA repair defects, confirming that the absence of ZNF280A is a key driver of the DNA repair defects in these cells, and that defective DNA repair is likely a major contributor to the clinical features observed in a subset of patients with 22q11.2 distal deletion syndrome.
The researchers believe future studies focusing on understanding how ZNF280A itself is regulated is necessary since understanding mechanistic nuances will be critical to establishing whether targeting ZNF280A could be a viable therapeutic option in diseases underpinned by genomic instability, such as cancer.
These findings appear online in the journal Nature Cell Biology.