Researchers Discover Protein Necessary for SARS-CoV-2 to Evade the Body’s Defenses
The human body is naturally equipped with defenses to fight off viral infections. For a virus to successfully infect it, it must first overcome these defenses. To do so, viruses have evolved specialized tools—proteins known as “virulence factors”—that help them shut down or dodge the immune system and cause disease.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, has an exceptional ability to overcome host defense barriers. It produces a set of specialized proteins that work together to overcome the human immune system, creating ideal conditions inside cells for the virus to multiply.
In a new study from Boston University Chobanian & Avedisian School of Medicine, researchers have identified a protein called non-structural protein 15 (nsp15) that plays a key role in helping SARS-CoV-2 hide from the body’s defenses by suppressing the production of viral double-stranded (dsRNA), leading to increased viral replication while limiting the body’s immune response.
“Out of the virus’s roughly 30 proteins, we found that nsp15 helps the virus control how much of its genetic material is visible in cells—essentially helping it fly under the radar of the immune system. By understanding how these viral proteins work, we can develop smarter ways to fight infections and design better treatments,” explains corresponding author Mohsan Saeed, PhD, associate professor of biochemistry and cell biology.
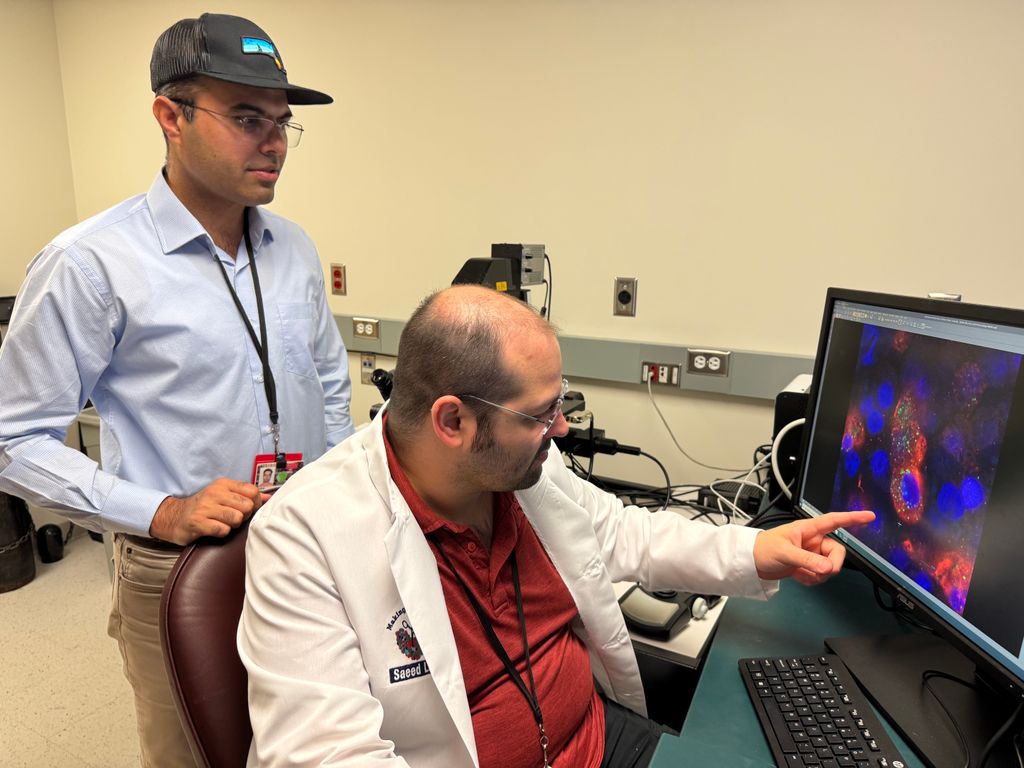 Dr. Saeed (left) and the first author Dr. Allen Caobi.
Dr. Saeed (left) and the first author Dr. Allen Caobi.
In an effort to understand how the SARS-CoV-2 nsp15 helps the virus to cause infection and disease, the researchers took three complementary approaches. First, they used human stem cell-derived lung cells that resemble those in the air sacs where COVID-19 often strikes. A modified virus lacking functional nsp15 grew poorly in these cells compared to the unmodified virus and was less able to block the cell’s natural defenses.
Next, they tested this modified virus in an experimental model engineered to carry the human receptor for the virus. While the unmodified virus caused severe disease and killed about 75% of the models, the modified virus caused milder illness, with only approximately 30% mortality.
Lastly, they studied a model that are naturally vulnerable to SARS-CoV-2. Those infected with the modified virus had lower levels of virus in their lungs and stronger immune responses compared to those infected with the unmodified virus.
“Together, these findings show that nsp15 plays a key role in helping SARS-CoV-2 grow, evade the immune system and cause serious disease,” adds Saeed, who also is an investigator at BU’s National Emerging Infectious Diseases Laboratories. “By revealing how nsp15 works, our findings open the door to designing antiviral drugs that target this protein and block infection. Such treatments are urgently needed, especially to protect people with weakened immune systems, who remain at high risk for COVID-19.”
According to the researchers, nearly all human coronaviruses have nsp15 or a closer version of it. Because these proteins are structurally so similar, they likely serve the same function in helping the virus spread and evade the immune system. “This makes nsp15 a promising target for antiviral drugs that could work not only against current coronaviruses but also future ones that may emerge. We are continuing to study nsp15 in hopes of designing powerful inhibitors that could one day become effective treatments.”
These finding appear online in the journal Proceedings of the National Academy of Sciences.