Personal Storytelling During Medical Training Improves Learning and the Way Doctors Connect with Their Patients
Medical Education
Personal Storytelling During Medical Training Improves Learning and the Way Doctors Connect with Their Patients
“By making space for personal stories in medical school, we aim to build a more human, compassionate healthcare system for everyone.”
Most medical schools teach students about illness through lectures or clinical vignettes as taught by doctors, but Boston University Chobanian & Avedisian School of Medicine offers a novel teaching experience whereby medical students share their own personal experiences with illness.
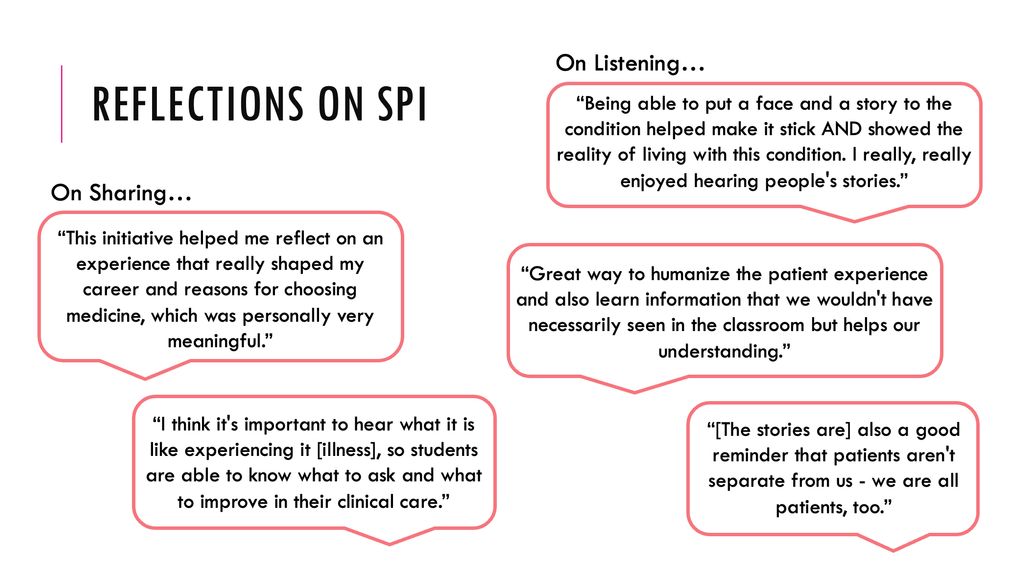
Recently, the school created the Student Perspectives Initiative (SPI), a student-led program where medical students share their own personal stories with illness that match topics being taught in class. For example, a lecture on inflammatory bowel diseases in the gastroenterology module would include a presentation by a student speaking about their own experience with Crohn’s disease.
In a new study, students who participated in the SPI program said that it helped them learn, understand the emotions connected to the disease, and feel more connected to each other. This is the first study demonstrating that storytelling by students themselves can be a lasting and meaningful way to improve medical education.
From 2020 to 2022, BU medical students learned basic science in their first year and clinical science in their second year. During the second year, students were introduced to SPI, where they shared personal stories matched to what they were learning in class. In 2023, BU changed the curriculum to combine basic and clinical science into one -and-a half years. Because of this, the SPI program was offered in both the first and second years.
Each year, approximately eight students gave voluntary presentations that lasted 30 to 60 minutes. Peer attendance was between 25 and 160 students. A faculty member also was present during the sessions to provide support and answer more technical questions related to anatomy and physiology. To measure the program’s impact, the researchers created a survey that asked about learning, empathy and community. They also asked for feedback to improve the program. Students could fill out the survey anonymously after the end of the SPI program, regardless of whether they had presented, attended or simply heard about the program.
 Ariel Hirsch, MD
Ariel Hirsch, MDAccording to the researcher, these findings show that a program like the SPI can help shape how future doctors learn to care for patients—not only by memorizing facts but by truly understanding what it feels like to be sick. “When medical students hear real stories from their peers about living with illness, they become more empathetic, emotionally aware and better prepared to support their patients. These kinds of experiences can lead to more compassionate, human-centered care in the long run,” explained senior author Ariel Hirsch, MD, professor of radiation oncology and director of radiation oncology education at the school.
 Elyse Olesinski, MD
Elyse Olesinski, MDThe researchers believe this study highlights the powerful idea that storytelling—especially personal storytelling—can be a tool for education, healing and connection. “It shows that when students share their own experiences with illness, it not only teaches important lessons but also helps build empathy and community. It also suggests that storytelling could be used more widely—not just in medicine, but in schools, workplaces, and communities—to help people better understand each other and grow together,” adds corresponding author Elyse Olesinski, MD, who graduated from the medical school in May and now is an internal medicine resident at Massachusetts General Hospital.
BU medical school graduate and founder of the program Seth Bergenholtz, MD, and current BU medical student Sarah Horn, also contributed to this study.
These findings appear online in the journal Medical Science Educator.