Immune System Genes Associated with Risk of Alzheimer’s Disease
A new study from an international collaboration of four institutions has identified three gene variants that contribute to the risk of developing Late Onset Alzheimer’s Disease (LOAD). All three genes–PLCG2, ABI3, and TREM2– are heavily expressed in microglia, a cell central to the brain’s immune system and its injury response system.
These findings appear in the journal Nature Genetics.
Researchers at Boston University School of Medicine, Cardiff University, University of Pennsylvania, University of Rotterdam and Institut Pasteru de Lille participated with over 30 other collaborators in an extensive three-stage genetic analysis of more than 85,000 subjects from several different AD genetic databases including the Framingham Heart Study.
In the first stage, genes from three separate databases and over 34,000 samples were sequenced. In the final two stages the variants identified in the first stage were analyzed against thousands of independent cases of AD and illness-free, control case genotypes. Ultimately, 37,022 cases of Alzheimer’s disease and 48,402 normal elderly controls from the Genetic and Environmental risk for Alzheimer’s Disease/ Defining Genetic, Polygenic and Environmental Risk for Alzheimer’s Disease (GERAD/PERADES) Consortium, Alzheimer’s Disease Genetic Consortium (ADGC), Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE), and the European Alzheimer’s Disease initiative (EADI) were used to power the study.
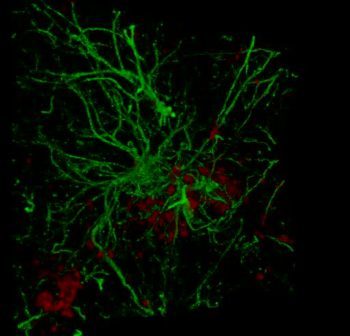 The study revealed three rare variants in the genes PLCG2, ABI3, and TREM2 that are each involved in the immune system response, especially in microglia, a cell which often acts as a first detect-and-respond, disposal system for harmful substances. “These genetic findings provide additional evidence that the innate immune response contributes directly to the development of Alzheimer’s disease,” explained corresponding author Sudha Seshadri, MD, professor of neurology at BUSM and FHS senior investigator.
The study revealed three rare variants in the genes PLCG2, ABI3, and TREM2 that are each involved in the immune system response, especially in microglia, a cell which often acts as a first detect-and-respond, disposal system for harmful substances. “These genetic findings provide additional evidence that the innate immune response contributes directly to the development of Alzheimer’s disease,” explained corresponding author Sudha Seshadri, MD, professor of neurology at BUSM and FHS senior investigator.
While it has been known since the 1980s that misfolded protein deposits, called beta-amyloid, found in the brains of decreased patients with AD are central to the cause of AD, recent experimental, genetic and epidemiological data has pointed to a more complex process involving the brain’s immune system in the progression of the disease. Emerging evidence now suggests that it is how the brain’s disposal system, the microglia, react to and handle the misfolded proteins that dictates disease formation and progression.
Key questions remain regarding the exact nature and at what stage microglial activation or inhibition is important in AD, however, this study provides a crucial link between specific genes and their potential role in the molecular progression of AD. The researchers hope that these advances in understanding the molecular inflammatory response in AD may lead to new potential targets for future therapies.
Submitted by Robert Simmons-Beck, MD.
This work was supported by the National Heart, Lung, and Blood Institute’s Framingham Heart Study (contracts N01-HC-25195 and HHSN268201500001I). This study was also supported by grants from the National Institute on Aging: AG033193, U01-AG049505, and AG008122 (S. Seshadri). S. Seshadri and A.L.D. were also supported by additional grants from the National Institute on Aging (R01AG049607) and the National Institute of Neurological Disorders and Stroke (R01-NS017950).
View all posts