Experiments utilizing burn wounds and implantation of polyvinyl sponges for preliminary and full experiments
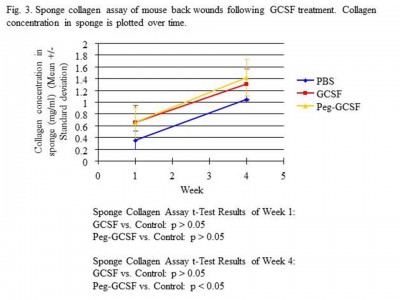
This is a proven model, developed many years ago. It is highly reliable, and capable of providing data on the accumulation of extracellular matrix proteins within the sponge, recruitment of cells from the area surrounding the sponge and/or from the peripheral circulation (if those cells are pre-labeled). The polyvinyl sponge has been thought of being a “wound” itself, and thus able to determine and monitor both local and systemic responses to therapeutic interventions. Fig. 4 shows an example of Dr. Falanga’s recent work when he tested the hypothesis that systemic administration of GCSF (for bone marrow mobilization) could lead to accelerated healing of both dorsal and full-thickness tail wounds. He did not find that to be the case, even over a range of GCSF concentrations. However, we did find a small increase in collagen accumulation in dorsally-implanted polyvinyl sponges in the GCSF-treated groups.