Overview of Program
Overview
The program is a world-class ABIM-accredited fellowship in Pulmonary Medicine and Critical Care Medicine that requires completion of three years to be board-eligible in both subspecialties.
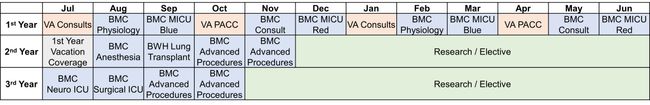
The first year follows a traditional clinical track that enables trainees to learn the requisite skills for the diagnosis and treatment of both common and rare diseases of the lung through rotations on the Pulmonary Consult and Pulmonary Acute Care Clinic (PACC) services at both Boston Medical Center (BMC) and the Veteran Affairs (VA) Boston Healthcare system. During the physiology rotation at BMC, trainees will gain exposure to management of extracorporeal membrane oxygenation (ECMO), pulmonary hypertension, and pleural disease and will be develop skills in right heart catheterization, chest thoracostomy, and advanced bronchoscopy (i.e., robotic bronchoscopy, endobronchial ultrasound). Lastly, trainees will acquire skills for the diagnosis and treatment of critically-ill patients through rotations on the two Medical Intensive Care Unit (MICU Blue and MICU Red) teams at BMC.
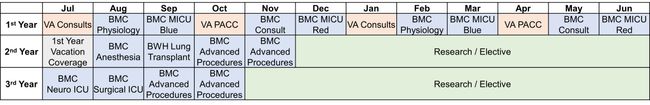
In the second and third years, trainees spend the majority of their time carrying out a mentored research project and gaining additional subspeciality clinical expertise. Required clinical rotations during second and third include Anesthesia, Neurological Intensive Care Unit (Neuro ICU), and Surgical Intensive Care Unit (Surgical ICU) during which trainees will also gain exposure to airway intubation, cardiopulmonary exercise testing (CPET), and bronchoscopy with endobronchial ultrasound (EBUS) (2 months during the second and third year). Trainees will also participate in an external rotation on the Lung Transplantation service at Brigham and Women’s Hospital.
In addition to required clinical rotations, there are a plethora of clinical electives available that can be used to personalize the schedule of third-year fellows interested in academic clinical careers. Trainees dedicated to research can choose to remain for a fourth year of protected research time to continue their mentored research project.
Personalizing your Training
 A key strength of the program is access to a wide array of outstanding clinical, educational, and research experiences. These broad experience options are used to individually tailor third year research and elective time to fit the career goals and interests of each trainee. There are numerous paths to success in our program. Many of our trainees devote their third years to:
A key strength of the program is access to a wide array of outstanding clinical, educational, and research experiences. These broad experience options are used to individually tailor third year research and elective time to fit the career goals and interests of each trainee. There are numerous paths to success in our program. Many of our trainees devote their third years to:
- Developing clinical expertise in specific content areas through clinical electives (see list below),
- Dedicated research time to write research grants and publish, and/or
- Gaining experience in clinical guidelines and professional society leadership (i.e., Faculty Kevin Wilson is Chief of Clinical Practice Guidelines and directs the Guideline Methodology Training Program for the American Thoracic Society and routinely includes trainees on writing committees and working groups).
More recently, the Department of Medicine has developed a multi-disciplinary median education sub-fellowship across the medicine fellowship programs. This novel program gives trainees in Pulmonary and Critical Care Medicine interested in medical education scholarship structured training in education, access to expert mentorship, and a diverse community of peers with shared goals.
Clinical Electives
- Additional Critical Care Training
- Median Intensive Care Unit Acting Attending
- Neurocritical Care Unit
- Surgical Critical Care Unit
- Additional Procedure Training
- Point-of-care Ultrasound (POCUS)
- EBUS
- Anesthesia Intubations
- Level 3 CPET
- Advanced Pulmonary Function Testing (High Altitude Simulation Testing [HAST], Methacholine Challenge, CPET)
- Additional Subspecialty Clinic
- Alpha-1 Center
- Amyloidosis Center
- Asthma and Allergic Diseases Program
- Bronchiectasis Program
- Center of Excellence in Sickle Cell Disease
- COPD and Chronic Respiratory Failure Program
- Interstitial Lung Disease Program
- Lung Nodule Program
- Pleural Diseases Program
- Pulmonary Rehabilitation Program
- Primary Immunodeficiency Program
- Pulmonary Hypertension Center (VA and BMC options)
- Sarcoidosis Center
- Sleep Disorders Center (VA and BMC options)
- Tobacco Treatment Center
- Tuberculosis Clinic
- Additional General Pulmonary Clinic
- VA PACC Acting Attending (Supervision of 1st year trainees)
- BMC Pulmonary Clinic Acting Attending (Supervision of 1st year trainees)
Call Schedule and Vacation
Weekend coverage is one weekend every six weeks for all the first and second year trainees. Third and fourth year trainees do not have weekend call responsibilities. Pulmonary and Critical Care Medicine service weekend coverage is provided by two attendings and two trainees. Weeknight call is pager call from home, with each trainee on call one night per week. There is no in-house call. Trainees will have 4 weeks of vacation each academic year during their fellowship training.
Moonlighting Opportunities
Trainees who are eligible to obtain a full Massachusetts state medical license may pursue moonlighting opportunities at BMC and other approved community sites at the beginning of their 2nd year of fellowship training. BMC, trainees who are board-eligible for Critical Care Medicine (i.e., 3rd year of fellowship training) may participate in the Special Care Unit Night Coverage (SCUNC) program provided that they have a full Massachusetts state medical license. The SCUNC program allows trainees to act as the overnight attending and oversee trainees in Internal Medicine in caring for patients admitted to both the MICU and the cardiac care unit (CCU).
 A key strength of the program is access to a wide array of outstanding clinical, educational, and research experiences. These broad experience options are used to individually tailor third year research and elective time to fit the career goals and interests of each trainee. There are numerous paths to success in our program. Many of our trainees devote their third years to:
A key strength of the program is access to a wide array of outstanding clinical, educational, and research experiences. These broad experience options are used to individually tailor third year research and elective time to fit the career goals and interests of each trainee. There are numerous paths to success in our program. Many of our trainees devote their third years to: