Inpatient Training
Fellows rotate between two hospitals, Boston Medical Center (BMC) and the Boston Veteran Affairs Medical Center (VAMC); together, these facilities provide rich and diverse clinical material. BMC, formed by the merger of Boston City Hospital and Boston University Medical Center Hospital, provides a unique clinical training ground for subspecialty training in pulmonary and critical care medicine. BMC has a long tradition of providing high quality care to indigent patients and continues to attract a large number of inner city, immigrant, and HIV-positive patients, consistent with its roots as Boston’s only public hospital. BMC also provides a full range of tertiary level medical care with active programs in thoracic oncology, solid organ and bone marrow transplantation, cardiac catheterization, and cardiac surgery. As a referral center for the entire New England region, the Boston VAMC provides trainees with the opportunity to direct the initial evaluation of lung cancer, manage severe airway diseases, and work-up a host of rare, infiltrative lung diseases.
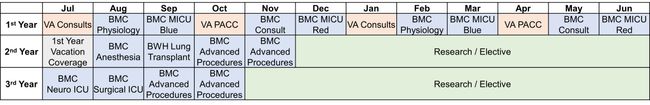
First year trainees rotate through six clinical rotations twice through the year. The clinical rotations and trainee responsibilities include:
Core Clinical Rotations
BMC Medical Intensive Care Unit (MICU)
This is a hands-on critical care rotation in which first-year trainees are dedicated to a 28-bed critical care unit. This is a busy, urban ICU where most patients are directly admitted from the emergency room and present with a wide array of acute problems. Under the supervision of the ICU attendings, trainees oversee care of critically ill patients and perform procedures. To facilitate their role as academicians, fellows are actively involved in the education of the medical house staff. Fellows lead daily “Vent Rounds” with the ICU respiratory therapist and critical care nurse. In this capacity, trainees expand their knowledge base of ventilator management and expedite the weaning of patients from the ventilator. Daytime intubations in the MICU may be performed by trainees under the guidance of anesthesiology. As third-years, trainees may return to the MICU as “Acting attendings” for a 4-week rotation on the MICU Green Team.
 |
 |
BMC Pulmonary Consult Service
In this rotation, the fellow is responsible for all in-patient pulmonary consultations and performance of all bronchoscopies. This includes inpatient and outpatient bronchoscopies as well as learning advanced bronchoscopy techniques including linear endobronchial ultrasound (EBUS), navigational bronchoscopy, and robotic bronchoscopy. On the consult service, fellows have the opportunity to see patients with a wide range of acute pulmonary problems, including a large number of international health problems (TB and other infectious diseases), pulmonary complications of HIV, sickle cell disease, and obstetric pulmonary problems. The fellow is also responsible for critical care consultative services to patients in the other critical care units of BMC including the Cardiac Care Unit (CCU) and Surgical Intensive Care Unit (SICU). Reflecting the tertiary level of care provided at Boston Medical Center, patients present with complex medical problems including pulmonary complications of bone marrow and solid organ transplantation, rheumatologic disorders, malignancy and chemotherapy related lung disease. In addition, there are active thoracic oncology, neurosurgery, cardiac surgery and interventional cardiology services, providing the fellow with a broad exposure to numerous complex, pulmonary problems typical of an academic medical center. Lastly, the fellow will also be reading and interpreting the pulmonary function tests performed daily at BMC, with attending supervision and education on the finer points of interpretation.
BMC Physiology Rotation
This main theme of the physiology rotation is the physiology of the the parenchymal, pleural, and vascular systems of the lung.
Pulmonary Hypertension Service: The Pulmonary Hypertension Center at BMC is a tertiary referral center for patients with a variety of pulmonary vascular diseases. Fellows on this rotation participate in the care of patients admitted to the Pulmonary Hypertension Service under the supervision of the Pulmonary Hypertension attending. This fellow also is part of a multidisciplinary Pulmonary Embolism Response Team (PERT). The pulmonary fellow along with a cardiovascular fellow see all PERT consults and facilitate the multidisciplinary discussion regarding the appropriate management of each patient presenting with an acute submassive/massive pulmonary embolism. The fellow on this rotation performs all the right heart catheterizations for patients undergoing evaluation for pulmonary hypertension. The pulmonary hypertension team performs more than 100 right heart catheterizations per year.
Pleural Service: The physiology fellow is responsible for the management of the Pleural Service patients. This rotation allows for a dedicated experience in diagnosing and managing disease of the pleura. This involves a dedicated pleural curriculum to review historical and contemporary literature surrounding pleural disease as well as procedural experience with thoracentesis, chest tube placement, and tunneled pleural catheter (Pleur-X) placement under the supervision of the Pleural Service attending. Pulmonary fellows on this rotation develop extensive experience with thoracic ultrasound.
Extracorporeal Membrane Oxygenation (ECMO): The physiology fellow will have an opportunity to be an integral part of the multidisciplinary ECMO team where they will assist in the care of patients requiring ECMO. The fellow will become familiar with the indications/contraindications of VA and VV ECMO and daily ventilator management.
VAMC Outpatient / Pulmonary Acute Care Clinic
VAMC Inpatient Consult / Procedures
This is a combined pulmonary and critical care medicine rotation. Fellows are responsible for consults on the inpatient medical service and performing outpatient bronchoscopies referred for this procedure by the Pulmonary Acute Care Clinic and continuity clinics. The first year fellows share approximately 200 bronchoscopies annually during this rotation. The Fellows are also responsible for providing critical care consultative services for patients in the surgical critical care and coronary care units of the Boston VAMC.
BMC Anesthesia Rotation
Second year fellows continue their critical care training during a month long rotation on the anesthesia service. The intent of this rotation is to develop a proficiency in elective and emergent airway management, use of double lumen endotracheal tubes and tube blockers, preoperative pulmonary assessment, and line placement. The fellows are instructed in preoperative clinical assessment related to anesthesia for elective and emergent surgery. There is formal instruction on induction agents, muscle relaxants, opiates, and inhalational agents. The fellows are instructed on the use of medications for conscious sedation. Fellows also spend time in the Post-Anesthesia Care Unit to gain experience in managing the types of problems that occur immediately following surgery. Fellows also attend anesthesia meetings, lectures, and Grand Rounds during this rotation. Fellows also have the opportunity to hone critical care ultrasound skills working with the critical care anesthesia team during this rotation. Fellows also receive additional airway skill development through the Pulmonary Fellow Airway course conducted in the Solomont Simulation Center.
BWH Lung Transplantation Rotation
Second year pulmonary and critical care medicine fellows rotate for a month on the Lung Transplantation Service at the Brigham and Women’s Hospital. During this rotation, pulmonary fellows have the opportunity to work with patients who are being evaluated for lung transplantation and those who have undergone lung transplantation. Fellows learn about the proper care of lung transplant patients, along with the potential complications that may occur. Fellows learn about the long-term complications faced by lung transplant patients such as rejection, infection, malignancy or deteriorating lung function. Fellows are participating in bronchoscopies performed to assess for infection as well as rejection. During this rotation, fellows develop a better understanding of the immune suppression used for lung transplant patients. Fellows also have an opportunity to assist in the critical care management of a newly transplanted patient on mechanical ventilation.
BMC Neuro ICU
Third year fellows continue to expand their clinical expertise by spending a 1 month rotation with the neurocritical care service. The Boston Medical Center neurocritical care service treats 500-600 patients a year with diverse diagnoses including subarachnoid hemorrhage, large territory stroke, hemorrhagic stroke, status epilepticus, neuromuscular emergencies, CNS infections, CNS tumors, and post-operative neurosurgical patients. Fellows have the opportunity to manage these critically ill patients under the guidance of board-certified fellowship-trained neurointensivists.
BMC Surgical ICU (SICU)
Third year fellows continue their critical care training by spending 1 month in the surgical intensive care units of Boston Medical Center as critical care fellows. This unique clinical experience takes advantage of the fact that Boston Medical Center is a Level I trauma center, with 28 SICU beds, and 1544 trauma admissions a year. In this capacity, Boston Medical Center is a receiving facility for the Boston Medflight Program, which is the main air evacuation system for this region. The critical care staff is board certified by The American Board of Surgery, Internal Medicine, and/or Anesthesia, and Critical Care. During this rotation, our fellows are directly involved in the care of severely injured patients, gaining the skills necessary to care for trauma victims. In addition to trauma, our fellows are involved in the care of orthopedic, general surgical, neurosurgical, and vascular patients that are admitted to the surgical intensive care unit. Boston Medical Center has begun an ECMO program for the management of complex cardiac surgery and medical patients. Pulmonary and critical care fellows have the opportunity to work with the multidisciplinary team of cardiac surgeons, pulmonologists, and cardiology to care for critically ill patients requiring ECMO support.
BMC Advanced Procedures Call
Cardiopulmonary Exercise Testing (CPET): Fellows rotate through the CPET lab during the second and third years. In this capacity, they are responsible for assessing the appropriateness of the indication for CPET, as well as the evaluation, execution, and analysis of the study. Fellows review each CPET on an individual basis with a supervising attending. The educational goals of this rotation include becoming familiar with the indications and contraindications for CPET, determining the impact of co-morbid medical conditions on exercise physiology, and the utilization of CPET for pre-operative assessment for patients prior to thoracic surgery.
Endobronchial Ultrasound (EBUS): Fellows will gain significant hands-on experience from performing Endobronchial Ultrasound (EBUS) procedures, which are crucial in diagnosing and staging lung cancer, as well as evaluating mediastinal and hilar lymphadenopathy. Fellows will learn to operate the EBUS bronchoscope, which combines traditional bronchoscopy with ultrasound technology gaining proficiency in navigating the airways, identifying key anatomical structures, and using ultrasound to visualize lymph nodes and masses. Fellows will practice fine-needle aspiration (FNA) of mediastinal and hilar lymph nodes, which is important not only for cancer staging but also for diagnosis of other conditions like sarcoidosis or other chronic infections. They will also be able to participate in multidisciplinary discussions by collaboration with pathologists, thoracic surgeons, and oncologists gaining insights into multidisciplinary care and decision-making.
Robotic-assisted Navigational Bronchoscopy: Fellows will gain valuable experience with robotic-assisted navigational bronchoscopy, which enhances their skills in diagnosing and managing lung lesions, especially in hard-to-reach areas of the lung. Fellows will become proficient in the use of robotic platforms that offer greater precision and stability compared to conventional bronchoscopy, allowing for more accurate access to peripheral lung nodules. They will learn to navigate complex bronchial pathways using virtual 3D models of the patient’s lungs created from CT scans, which assists in targeting small or difficult-to-reach lesions that are typically inaccessible with traditional methods. Fellows will perform biopsies of peripheral lung nodules or masses with enhanced accuracy due to the robotic system’s ability to maintain a stable platform for needle insertion, improving diagnostic yield, particularly for early-stage lung cancer. They will use real-time imaging modalities, such as fluoroscopy, electromagnetic navigation, and cone-beam CT, to confirm the precise location of the biopsy tool and enhance procedural safety. By participating in these procedures, fellows will gain experience in evaluating which patients are suitable candidates for robotic bronchoscopy, managing procedural risks, and integrating biopsy results into broader patient care plans, particularly in collaboration with oncologists, thoracic surgeons, and radiologists.