Trainee, Visitor and Volunteer Onboarding
Johnson & Johnson expands project that aims to predict, prevent diseases
March 22, 2016 | Written By: Tribune news services | Source: ChicagoTribune
Johnson & Johnson has ramped up its ambitious project to learn how to predict who will develop particular diseases and find therapies to prevent or stop the disease early, when it's most treatable.
Since the health care giant announced its groundbreaking project in February 2015, it's expanded to include two dozen research programs with partners — in government, universities, patient advocacy groups and other drug and diagnostic test companies. Their expertise and resources should speed discoveries and allow Johnson & Johnson to spread its funding across more ventures.
On Tuesday, J&J gave an update and announced the latest two projects. They're meant to identify which pregnant women will develop gestational diabetes, and to identify and treat people at risk of or in early stages of chronic obstructive pulmonary disease, the third-leading cause of death worldwide.
"We've really been trying to introduce a new paradigm," the J&J project head, Ben Wiegand, told The Associated Press in an exclusive interview. "We're moving from disease care to health care."
Wiegand said the mapping of the human genome and other recent scientific advances have made that goal feasible. J&J's "Disease Interception Accelerator" now is working on multiple studies in Type 1 and gestational diabetes, cataracts and vision-damaging presbyopia, depression in women during and after pregnancy, lung disorders and cancers of the cervix, mouth and throat caused by human papilloma virus.
The project is remarkable in an industry whose bread and butter is medicines that patients with chronic diseases take for years.
The idea is to first discover biomarkers — measurable biological and molecular signs in blood and other patient samples — indicating a disease will develop or is beginning. Next, scientists would develop affordable and easy-to-use diagnostic tests for those biomarkers.
Finally, researchers would develop new therapies, or determine which existing ones would work, to head off full-blown disease in those people. Those could include medicines, nutrition changes and physical or psychological therapy.
If successful, those strategies could be used much as cholesterol tests are given to patients, with those who have a problem being prescribed statin drugs to prevent a heart attack or stroke.
"This is the way to go," said Dr. Robert Hardi, president of the Academy of Physicians in Clinical Research. "If anybody can pull it off, they can" — with help from partners.
He noted that researchers already are developing biomarker tests in areas such as cancer that help doctors pick the best treatment for each patient.
"It may well save a lot of money and a lot of suffering," added Hardi, a gastroenterologist in Chevy Chase, Maryland.
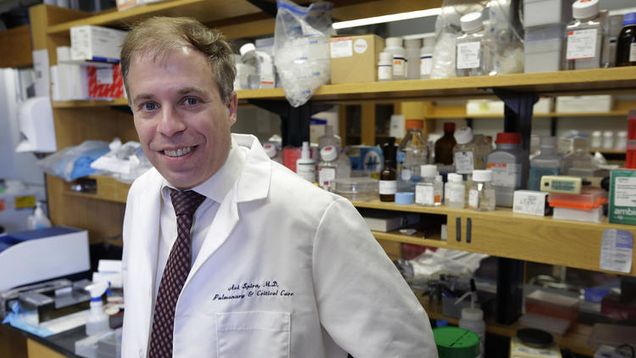
One of the newest projects piggybacks on existing research at Boston University School of Medicine. It's been working since 2011 under a Defense Department grant to identify which military members and veterans will develop lung cancer. That group has a high risk because many are heavy smokers and they're exposed to fuel fumes and other dangerous substances while deployed, said Dr. Avrum Spira, a pulmonologist heading that study.
It's been testing blood and skin cells and doing chest scans on hundreds of participants, aiming to link changes in those tests over time to which people later develop lung cancer. J&J has given Spira's group $8 million to test 1,000 civilian smokers, to identify cell changes in the individuals who eventually develop chronic obstructive pulmonary disease, which includes emphysema and chronic bronchitis. They'll then test therapies to stop further destruction of lung airways.
With another $2.1 million from J&J, Spira said, his team is studying how the immune system fails in the early development of lung cancer and whether new drugs that fight cancer by boosting the immune system could prevent it.
Another new collaboration is seeking biomarkers indicating which pregnant women likely will develop gestational diabetes, so they can be treated to prevent it. Half those women would otherwise develop Type 2 diabetes within 10 years, and their babies have an eightfold risk of developing it eventually, Wiegand said.
Preventing diseases or treating them early on is much cheaper than trying to save people diagnosed with advanced disease, so Wiegand believes that insurers will cover the diagnostic tests being developed and new, proven treatments.
Johnson & Johnson, based in New Brunswick, New Jersey, is a leading maker of diagnostic tests, as well as vaccines, surgical equipment and prescription medicines, putting it in a good position to offer products for many of the disorders being studied.
For the project to have a big impact, the U.S. must to address the shortage of primary care doctors, said Dr. Wanda Filer, president of the American Academy of Family Physicians. She said pediatricians, family doctors and internists, along with nurse practitioners, already focus on preventive care such as vaccines, so they're best suited for identifying and helping at-risk patients.
With patients more focused on medical costs as they bear more of them now, Filer said, they'll need to be convinced new diagnostic tests and pre-emptive treatment are worth the cost.
"This could be transformational," she added.
For additional press, please visit this site: BUSM
Stopping Lung Cancer Before It Gets Going
March 7, 2016 | Written By: Upal Basu Roy, MPH, PhD | Source: LUNGevity
“The LUNGevity award provided me the resources to study premalignant lung cells—a stage in which normal lung cells have changed, but not yet completely into cancer cells. This is an extremely important area of cancer research for lung cancer as well as for other types of cancers. Studying premalignant cells provides us a unique window to understand the early stages of lung cancer—before the lung cells acquire the mutations in DNA that allow them to become cancer cells. Such studies allow us not only to develop biomarkers for early disease detection, but also to identify new targets for cancer treatment and prevention.” —Jennifer Beane, PhD
Cancer develops in a sequenced manner. Patches of lung cells gain the ability to multiply faster than their neighboring normal cells by acquiring mutations. These patches of cells are called “premalignant lesions" (PMLs). Some of these lesions may eventually become cancer. LUNGevity Career Development Awardee Dr. Jennifer Beane from Boston University has been studying the differences between PMLs and normal lung cells in order to develop predictive biomarkers to determine who might be at high risk for developing lung cancer and thus need further screening. I sat down with her to discuss her work.
LUNGevity: What is the focus of your LUNGevity award?
Jennifer Beane: I was always interested in developing tools to catch lung cancer early. As a PhD student, I studied how a special type of cell that lines the respiratory tract, also known as a respiratory epithelial cell, reacts to cancer-causing substances, or carcinogens. As you know, exposure to cigarette smoke is a known risk factor for lung cancer. My project focused on understanding how smoking injures respiratory epithelial cells. I helped develop a biomarker that could identify whether or not epithelial cells were from a person with lung cancer. While this was exciting, I became interested in understanding earlier stages of the disease—what are the changes that are happening in normal lung cells before they become cancerous? I wanted to learn more about this stage because it represents a unique opportunity for therapeutic intervention. That’s how I got interested in the study of premalignant lesions, or PMLs. These patches of cells in the respiratory tract are not like normal lung cells. They have a life of their own. They can progress quickly to become cancer, go away, or stay stable for years without causing any trouble. What determines whether these lesions become cancerous? Does how the cells respond to injury from carcinogens decide whether a PML becomes cancerous? These questions keep me awake at night and are the focus of my LUNGevity grant. With this grant, I am studying RNA molecules from normal lung cells and PML cells to understand how they work and then develop a biomarker that can identify the presence of PML cells and predict which PMLs will progress to full-blown cancer.
L: What are some of the major findings of your project?
JB: Cells in our body use different metabolic pathways to make energy. While studying PMLs, we stumbled upon something unusual: PMLs and normal lung cells use different pathways to produce energy and survive. We can capture this difference and other changes in a biomarker signature that I developed. This is helpful because our technology is easily adaptable to a clinical setting. In the clinic, respiratory cells are collected during a procedure called bronchoscopy. These cells can then be tested for the presence of a precancer signature. Veracyte, a biotechnology company, has already developed a test known as PerceptaTM to decide whether a person needs further invasive tests to diagnose lung cancer. The idea behind the research on PMLs is to develop similar such tests that can identify people with PMLs that will progress to cancer. People with these types of PMLs would need more aggressive screening or may benefit from cancer prevention drugs. This is a very exciting time in early detection research because there are so many new technologies.
L: How is your project changing our understanding of chemoprevention for lung cancer?
JB: Our research has opened up the exciting possibility of developing drugs that stop lesions from progressing to full-blown lung cancer, a concept known as chemoprevention. For example, taking an aspirin can protect you from developing colon cancer if you belong to the high-risk group. However, we have not had much success with chemoprevention in lung cancer. This might have been because we were not selecting the right group of patients. Now that we have a biomarker signature for PML, we can use it to select patients who might benefit from chemoprevention and treat them with a drug that stops cancer from developing. We are not there yet, but I cannot help but feel excited—we might someday have drugs that stop lung cancer from developing altogether.
(This is the first blog in a two-blog series of interviews with our amazing women scientists, who are contributing to major progress in lung cancer research. Stay tuned for the next blog, which will be focused on Targeted Therapy.)
How RNA Editing May Promote Tumor Growth
Thursday, March 17 2016 | Source: BUSM
A new study provides insight on the potential role played by RNA (ribonucleic acid) editing in cancer.
The findings, which appear online in the journal Scientific Reports, may further our understanding of an emerging mechanism implicated in tumor initiation and progression, and may thus lead to the development of better treatment options in the future.
In every healthy human cell, the genetic information hard-wired into the DNA is transcribed into messenger RNA, which is in turn translated into proteins, the workhorses of all body tissues and organs. The prevailing view is that most malignancies are caused by DNA mutations, which can lead to the aberrant activation or inactivation of the corresponding protein products and to the consequent out-of-control growth and proliferation of malignant cells. RNA editing, the process by which ‘mutations’ of the RNA sequence are introduced post-transcriptionally, has the potential to impact a variety of cellular processes yet the precise mechanism of how has been poorly understood until now.
Previous studies have shown that more than one million sites in the genome are edited to various degrees. Despite the fact that a majority of these editing sites fall within regions that are not translated to protein, it has been shown that the differences in RNA editing levels between tumor and normal tissues are associated with different clinical outcomes. Currently, only a few coding RNA editing sites have been functionally characterized. However, it is still a puzzle whether and how the majority of the RNA editing events in the untranslated regions affect tumor growth.
Researchers from Boston University School of Medicine (BUSM) analyzed 14 tumor types, and identified more than 2,000 genes showing significant changes in RNA editing level between tumor and normal tissues.
“This study suggests that RNA editing may serve as an important epigenetic mechanism of cellular regulation beyond the genetic/DNA level,” explained corresponding author Stefano Monti, PhD, associate professor of medicine at BUSM. “We show that the effect of one epigenetic component can be offset by changes in another epigenetic component. Thus, it is important to have a comprehensive picture of changes in the cancer genome, which may point to vulnerabilities amenable to targeted treatment,” added lead author Liye Zhang, PhD, postdoctoral fellow at BUSM.
Funding for this study was provided by the MGHPCC Seed Fund program, the Evans Center for Interdisciplinary Biomedical Research ARC on “Etiology and Pathogenesis of Oral Cancer (EPOC)”, and the NIH National Heart Lung and Blood Institute (1R01HL124392-01).
New test could sharply reduce risky, costly lung cancer biopsies
Press Release: May 18, 2015 | Written by Lenny Bernstein - The Washington Post
When a suspicious lesion shows up in the lungs on a CT scan, the first thing your doctor wants to know is whether it's cancerous. A specialist will pass a long, thin bronchoscope into your airway in the hope of grabbing a few cells of the growth so they can be examined under a microscope.
But some of these lesions or nodules are deep in the small branches of the lungs, out of reach of the bronchoscope, which is about the diameter of a pen. Other times, the results are inconclusive. That has left only two ways to determine whether the abnormality is cancerous: inserting a needle through the chest wall and into the tumor, or surgically opening a patient's chest to find it (and remove it if necessary).
The first procedure carries a 15 percent risk of collapsing a lung (pneumothorax), as well as infection. The second is serious surgery that requires general anesthesia and results in the loss of lung tissue. Both are in-patient procedures that carry the cost and other risks of hospitalizations. In about a third of the surgeries, the growth turns out to be benign, meaning the surgery was unnecessary.
But now, according to a study published Sunday in the New England Journal of Medicine, there appears to be a new, much less invasive way of determining whether a growth is malignant. Researchers at Boston University have discovered that the thin epithelial cells that line the entire airway show changes that indicate whether a growth is malignant. With small brushes on the bronchoscope, they can take some of those cells and, using genomic testing that has been available only in recent years, reach a conclusion.
The study released Sunday showed that the tests were about 97 percent accurate on 639 subjects. A private company has purchased the technology and is making it available to hospitals across the country.
"Even though lung cancer tends to develop deep in your lung, all the cells that line your airway are exposed," said Avrum Spira, a professor of medicine at Boston University who led the research. "They have changes in their genome."
Spira's test focuses on messenger RNA, the molecules that express genes' instructions to cells. He called the technology "a canary in the coal mine" for lung cancer, which kills about 160,000 people in the United States each year.
If the test is negative, its accuracy will allow doctors to wait and watch a lesion. If it shows a malignancy, a biopsy still would be needed to confirm the cancer. "There will still be a small number of biopsies," Spira said. "But we're going to reduce them significantly."
Other research is being conducted to find markers for lung cancer, though much of it focuses on substances that can be found in the blood, Spira said. With the vast majority of lung cancer victims being smokers, the epithelial cells show changes that could be tracked once the technology became available, he said.
The next logical question is whether those changes might be detected early enough to predict and prevent lung cancer. Spira said his team already is working on research to determine whether that's possible.
The current advance was a long time in coming and shows the difficulty of bringing research from the lab to the consumer. Spira said the initial discovery was made 12 years ago, but he couldn't find any private group willing to put up the millions of dollars needed to conduct studies, work through the government and academic regulatory process and bring his idea to market.
Seven years ago, he formed his own company, raised venture capital and eventually proved that his idea worked. Now his company has been purchased by Veracyte, which will take over the production and marketing of the "Bronchial Genomic Classifier."
"We were adding 30 seconds to a minute" to the length of a bronchoscopy, Spira said. ". . . Even then, the regulatory hurdles were significant. We got over them all, but they were significant."
Veracyte Initiates Launch of Percepta™ Bronchial Genomic Classifier
Press: April 16, 2015 | Veracyte
South San Francisco, Calif. --- April 16, 2015 --- Veracyte, Inc. (NASDAQ: VCYT), a molecular diagnostic company pioneering the field of molecular cytology, today announced the launch of its Percepta™ Bronchial Genomic Classifier, a new genomic test to resolve ambiguity in lung cancer diagnosis. The company will soon begin testing patient samples in its CLIA-certified laboratory, with the Percepta test now available to a limited number of institutions around the country.The Percepta test is designed to reduce the number of invasive biopsies and other procedures that can follow when suspicious lung nodules are found on computerized tomography (CT) scans. The test is used when results from a bronchoscopy – a common nonsurgical procedure to evaluate lung nodules – are non-diagnostic, meaning that cancer cannot be ruled out. Data from a prospective, multicenter clinical validation study previously demonstrated the Percepta test's ability to identify patients whose lung nodules are at low risk of malignancy so that they can be monitored with CT scans in lieu of invasive diagnostic procedures.
"Our Percepta test can help patients avoid unnecessary, potentially risky procedures while simultaneously reducing the growing cost burden associated with lung cancer diagnosis," said Bonnie H. Anderson, Veracyte's president and chief executive officer. "We believe the clinical and public-health need for the Percepta test becomes even greater as more patients become eligible for new lung cancer screening programs."
Ms. Anderson noted that, beginning in early 2015, more than eight million Americans at high-risk for lung cancer became eligible for annual screening with low-dose CT (LDCT) through new private-insurer and Medicare coverage requirements.
"Bronchoscopy is attractive to clinicians and patients because it offers a nonsurgical method for diagnosing suspicious lung nodules. However, given the difficulty in accessing small peripheral nodules, it often produces non-diagnostic results, leaving clinicians with the dilemma of whether to subject patients to invasive and potentially unnecessary diagnostic procedures or just monitor them with CT scans, with the risk that they may have cancer," said Avrum Spira, MD, M.Sc., professor of medicine at Boston University and co-developer of the genomic test. "The Percepta test can help determine a lung nodule's likelihood of cancer, without the need to sample the nodule directly, which should provide very tangible benefits to patients, medical professionals and the healthcare system."
Veracyte's test comprises a 23-gene molecular classifier that uses proprietary "field of injury" technology to detect molecular changes that occur in the epithelial cells lining the lung's respiratory tract in response to smoking — the cause of 85-90 percent of lung cancers. These changes can be detected in cells obtained from standard cytology brushings taken during bronchoscopy from the proximal airway, and indicate the presence of malignancy or disease processes from distant sites in the lung.
An estimated 250,000 patients currently undergo a bronchoscopy each year in the U.S., with approximately 40 percent producing non-diagnostic results. These numbers are expected to increase significantly with the new insurance coverage requirements for annual CT screening. Veracyte noted that it does not expect meaningful revenue from the Percepta test until 2017.
About Veracyte
Veracyte (NASDAQ: VCYT) is pioneering the field of molecular cytology, focusing on genomic solutions that resolve diagnostic ambiguity and enable physicians to make more informed treatment decisions at an early stage in patient care. By improving preoperative diagnostic accuracy, the company aims to help patients avoid unnecessary invasive procedures while reducing healthcare costs. Veracyte's first commercial solution, the Afirma® Thyroid FNA Analysis, centers on the proprietary Afirma Gene Expression Classifier (GEC) to resolve ambiguity in diagnosis and is becoming a new standard of care in thyroid nodule assessment. Since launching its Afirma solution in 2011, Veracyte estimates it has helped approximately 15,000 patients with thyroid nodules avoid unnecessary surgery, reducing healthcare costs by millions of dollars. The Afirma test is recommended in leading practice guidelines and is covered for 145 million lives in the United States, including through Medicare and many commercial insurance plans. Veracyte intends to expand its molecular cytology franchise to other clinical areas, beginning with difficult-to-diagnose lung diseases. In April 2015, the company launched the Percepta™ Bronchial Genomic Classifier, a test to resolve preoperative ambiguity in lung nodules that are suspicious for cancer. Veracyte is also developing a second product in pulmonology, targeting interstitial lung diseases, including idiopathic pulmonary fibrosis. For more information, please visit www.veracyte.com.
Behind the Vapor – Chasing the facts behind e-cigarette health risks
Press: October 20, 2014; written by Sara Rimer | BU Research
With the public health community sharply divided over the potential benefit and harm of the popular device—and with conclusive scientific evidence in short supply—the World Health Organization (WHO) released a report in August 2014 that raised serious questions about the health impact of e-cigarettes and called for a ban on indoor use and sales to minors. The report expressed “grave concern” over the growing role of multinational tobacco companies, warning that they could turn e-cigarettes into a gateway for a new generation of smokers at a time when a decades-long public health campaign has successfully reduced smoking rates in the US and other developed countries.
Also in August 2014, the Centers for Disease Control (CDC) reported that more than a quarter million youth who had never smoked a cigarette used e-cigarettes in 2013, three times the number of users since 2011. The Food and Drug Administration (FDA) proposed bringing e-cigarettes under its control alongside tobacco in the spring of 2014, but that proposal is enmeshed in debate and lawsuits. Dozens of states and cities across the country, including Boston, have already banned the use of e-cigarettes indoors.
At Boston University, Avrum Spira (ENG’02), a pulmonary care physician and School of Medicine associate professor of pathology and laboratory medicine and bioinformatics who studies genomics and lung cancer, was one of the first scientists to receive funding from the FDA to investigate the health effects of e-cigarettes. “In theory—and how they’re marketed—e-cigarettes are a safer product because they don’t have tobacco, which has known carcinogens,” Spira says. “The question is: does safer mean safe?”
Across BU’s Medical Campus from Spira, Michael Siegel, a physician and professor of community health sciences at the School of Public Health, has emerged as perhaps the country’s most high-profile public health advocate for e-cigarettes. Siegel, who is not currently researching e-cigarettes, says he believes that the device could potentially help large numbers of smokers quit, or drastically decrease, a habit that is the leading cause of preventable deaths in the US. He points out that despite all the existing smoking cessation products on the market, only a small fraction of cigarette smokers manage to quit. Only 4 to 7 percent break the habit without some nicotine replacement or medication, according to the American Cancer Society. At the same time, Siegel says, more research is needed on the health effects of e-cigarettes as well as their effectiveness in helping people quit smoking.
To read more on the interviews with Drs. Spira and Siegel please visit this BU Research site.
Researchers will study relation of environment to breast cancer
Press: October 16th 2014, written by Todd Feathers | Boston Globe
Five eminent Boston researchers will officially join forces Thursday to tackle one of the most perplexing questions about breast cancer: Why do so many people with no family history of the disease get it?
The researchers will examine whether common man-made chemicals are responsible for the disease, which increasingly strikes men and women.
In 2014, breast cancer will be the second-most-diagnosed form of cancer and the third- deadliest form of the disease, according to the National Cancer Institute. But unlike with some other cancers, the vast majority of breast cancer diagnoses — more than 90 percent — cannot be traced to a hereditary cause, the institute said.
“I think what we’re going to be doing is adding the weight of evidence that environmental chemicals contribute significantly to [breast] cancer, more than most people expect,” said David H. Sherr, of the Boston University School of Public Health. He is leading the team.
The research is backed by a three-year, $5 million grant from ART beCAUSE, a breast cancer foundation.
Ellie Anbinder, its cofounder, spearheaded the funding effort. She survived breast cancer but was left wondering why she developed it in the first place.
“The bottom line is that there is not a lot of coordinated research around the environment and breast cancer,” she said. “We felt that in order to have some kind of strong impact on the field of environmental causes of breast cancer we needed to put together a large project.”
Most cancer research is dedicated to developing drugs or cures, Sherr said. But the Boston consortium’s ultimate goal is finding a way to prevent the cancer from ever taking hold.
Sherr studies receptors in cells that detect chemicals in their vicinity. Fellow researchers Gail Sonenshein, of Tufts University School of Medicine, and Dr. David C. Seldin, of the Boston University School of Medicine, will examine signaling pathways that tell a cell when and how to change once it interacts with a chemical.
Charlotte Kuperwasser, also of Tufts, is a pioneer of the theory of cancer stem cells.
Rounding out the team is Stefano Monti, of BU, a computational biologist who uses algorithms to project how cells will react to certain chemicals.
Veracyte to Acquire Allegro Diagnostics: Plans to Launch Lung Cancer Test
Press release: September 4th 2014
SOUTH SAN FRANCISCO, Calif., Sept. 4, 2014 /PRNewswire/ -- Veracyte, a molecular diagnostics company pioneering the field of molecular cytology, today announced an agreement to acquire Allegro Diagnostics Corp. based in Maynard, Mass., for $21.0 million, comprised of $7.8 million in cash and $13.2 million in Veracyte common stock. Allegro is a privately held company focused on developing genomic tests to improve the preoperative diagnosis of lung cancer.
Veracyte plans to commercially launch Allegro's lead lung cancer test in the second half of 2015, with meaningful revenue expected in 2017.
Allegro's lung cancer test is designed to help physicians determine which patients with lung nodules who have had a non-diagnostic bronchoscopy result are at low risk for cancer and can thus be safely monitored with CT scans rather than undergoing invasive procedures. The gene expression test uses Allegro's proprietary "field of injury" genomic technology platform to circumvent the traditional challenge of obtaining accurate lung nodule samples for testing, without surgery or other invasive, risky and expensive procedures.
"With Allegro and its novel, clinically validated lung cancer test, we plan to accelerate our entry into the pulmonology market, enabling us to improve care for patients with lung nodules while creating long-term growth opportunities," said Bonnie H. Anderson, Veracyte's president and chief executive officer. "Allegro is a natural fit for us and we believe this move further establishes our leadership in molecular cytology, using genomics to resolve diagnostic ambiguity preoperatively and thus spare patients from unnecessary invasive procedures and reduce associated healthcare costs."
Allegro's technology detects molecular changes that occur throughout the respiratory airways in response to smoking – the cause of almost all lung cancers – and that are correlated with disease. These changes can be detected in a gene expression signature from cytologically normal airway cells and indicate the presence of malignancy or disease processes from distant sites in the lung. The lung cancer test is performed on cytology samples obtained through bronchoscopy, a minimally invasive procedure that enables a physician to access airways in the lung. The molecular classifier's performance has been established in two prospective, multicenter clinical validation studies, involving 25 centers and nearly 1,000 patients.
"We are excited for our lead test to become available to patients, helping to reduce unnecessary diagnostic surgeries and other procedures among the hundreds of thousands of patients with lung nodules who undergo bronchoscopies each year in the U.S to rule out cancer," said Michael D. Webb, president and chief executive officer of Allegro Diagnostics. "We believe Veracyte is uniquely poised to commercialize and gain reimbursement for our test, given the rapid success the company has achieved with its Afirma® solution in endocrinology."
About Lung Cancer Diagnosis
Lung cancer is the leading cancer killer in the U.S., with an estimated 225,000 new cases diagnosed and approximately 160,000 deaths caused by the disease each year. Recent guidelines recommend annual CT screening for high-risk patients, with an estimated eight million Americans falling into this category based on smoking history and age. Among the approximately 250,000 bronchoscopies currently performed each year in the U.S. to evaluate lung nodules – a potential sign of cancer – up to 40 percent produce non-diagnostic results, based on pathology. Approximately half of these patients undergo surgery or other invasive procedures to obtain a diagnosis. Data show that approximately 40 percent of lung nodule patients who undergo surgery prove to have benign nodules. Thus, a better way to risk-stratify patients at high risk of lung cancer could help determine which patients can be safely followed with CT scans versus invasive procedures.
About Veracyte
Veracyte is pioneering the field of molecular cytology, focusing on genomic solutions that resolve diagnostic ambiguity and enable physicians to make more informed treatment decisions at an early stage in patient care. By improving preoperative diagnostic accuracy, the company aims to help patients avoid unnecessary invasive procedures while reducing healthcare costs. Veracyte's first commercial solution, the Afirma® Thyroid FNA Analysis, provides a comprehensive approach for assessing thyroid nodules, centered on the proprietary Gene Expression Classifier (GEC) to resolve ambiguity in diagnosis. Each year, of the more than 525,000 thyroid nodule FNAs performed in the U.S., approximately 115,000 patients undergo diagnostic thyroid surgery, with 70% to 80% of nodules proving benign and thus the surgery unnecessary. Veracyte commercially launched Afirma in January 2011. As of June 30, 2014, the company has received nearly 115,000 FNA samples for evaluation using Afirma and has performed over 20,000 GECs to resolve indeterminate cytopathology results. Backed by multiple, peer-reviewed, published studies and included in leading medical guidelines, Afirma is covered by Medicare and major commercial payers, which collectively represent more than 135 million covered lives. Afirma is marketed and sold through a global co-promotion agreement with Genzyme Corporation, a subsidiary of Sanofi. Veracyte intends to expand its molecular cytology franchise to other clinical areas and is in product development for its first product in pulmonology. For more information, please visit www.veracyte.com.
Forward-Looking Statements
This press release contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995, including statements relating to the company's belief that the acquisition of Allegro will accelerate Veracyte's entry into the pulmonology market and allow it to improve patient care while creating long-term growth opportunities, the company's plans to launch Allegro's lung cancer test in the second half of 2015 and its beliefs regarding when it expects to derive meaningful revenue from the test, the company's beliefs regarding the benefits of its tests and Allegro's tests to physicians, patients and payers, and the company's intent to expand its molecular cytology business into other clinical areas. Forward-looking statements involve risks and uncertainties, which could cause actual results to differ materially, and reported results should not be considered as an indication of future performance. These risks and uncertainties include, but are not limited to: our ability to close the acquisition; our limited operating history and history of losses; our ability to increase usage of and reimbursement for Afirma and any future products we may develop or sell, including the Allegro lung cancer test; our ability to continue our momentum and growth; our dependence on a few payers for a significant portion of our revenue; the complexity, time and expense associated with billing and collecting from payers for our test; laws and regulations applicable to our business, including potential regulation by the Food and Drug Administration or other regulatory bodies; our dependence on strategic relationships and our ability to successfully convert new accounts resulting from such relationships; our ability to develop and commercialize new products and the timing of commercialization, including our ability to successfully commercialize the Allegro lung cancer test; our ability to achieve sales penetration in complex commercial accounts; the occurrence and outcome of clinical studies; the timing and publication of study results; the applicability of clinical results to actual outcomes; our inclusion in clinical practice guidelines; the continued application of clinical guidelines to our products; our ability to compete; our ability to expand into international markets; our success integrating Allegro into our business; our ability to obtain capital when needed; and other risks set forth in the company's filings with the Securities and Exchange Commission, including the risks set forth in the company's Quarterly Report on Form 10-Q for the quarter ended June 30, 2014. These forward-looking statements speak only as of the date hereof and Veracyte specifically disclaims any obligation to update these forward-looking statements.
Veracyte, Afirma, the Veracyte logo, and the Afirma logo are trademarks of Veracyte, Inc. This press release also contains trademarks and trade names that are the property of their respective owners.
Media:Tracy Morris
650-380-4413
Tracy.Morris@Veracyte.com
Investors:Angeli Kolhatkar
Burns McClellan, Inc.
212-213-0006
akolhatkar@burnsmc.com
New way to determine cancer risk of chemicals found
Press Release from July 24th 2014
A new study has shown that it is possible to predict long-term cancer risk from a chemical exposure by measuring the short-term effects of that same exposure. The findings, which currently appear in the journal PLOS ONE, will make it possible to develop simpler and cheaper tests to screen chemicals for their potential cancer causing risk.
Despite an overall decrease in incidence of and mortality from cancer, about 40 percent of Americans will be diagnosed with the disease in their lifetime, and around 20 percent will die of it. Currently fewer than two percent of the chemicals on the market have been tested for their ability to induce cancer.
Using an experimental model, researchers from Boston University School of Medicine (BUSM), Boston University School of Public Health, the BU Bioinformatics Program and the National Toxicology Program at the National Institute of Environmental Health measured the effects on healthy tissue from few days of exposure to a given chemical and assessed the effects on the gene expression response in the liver. "By comparing the responses to known chemical carcinogens and non-carcinogens, we were able to extract a "signature" and an associated predictive model capable of discriminating with high accuracy between the two," explained corresponding author Stefano Monti, PhD, associate professor of medicine at BUSM and a member of the BU Superfund Research Program. "Furthermore, by inspection of the coordinated set of genes driving the response to chemical exposure, we were able to zoom in to the potential mechanisms driving cancer induction," he added.
According to the researchers there is growing recognition that the role played by environmental pollutants in human cancer is under-studied and that more formal approaches to the analysis of the biological consequences of prolonged exposure to pollutants are needed. "This work has confirmed that it is possible to predict the long-term cancer risk by measuring the short term effects," said Monti. "As a result of our findings we expect that accurate and cost-effective screening for evaluating the carcinogenic potential of the more than the 80,000 chemicals currently in commercial use soon will be a reality."
Publication: Daniel Gusenleitner, Scott S. Auerbach, Tisha Melia, Harold F. Gómez, David H. Sherr, Stefano Monti. Genomic Models of Short-Term Exposure Accurately Predict Long-Term Chemical Carcinogenicity and Identify Putative Mechanisms of Action. PLoS ONE, 2014; 9 (7): e102579 DOI:10.1371/journal.pone.0102579
Story Source: The above story is based on materials provided by Boston University Medical Center. Note: Materials may be edited for content and length.
Links to additional press: Voice of America and Chemical Watch
BUSM Researchers Identify Molecule that Could Aid Lung Cancer Detection, Treatment
Press Release: From October 28th 2013
Written by Jenny C Leary
Researchers at Boston University School of Medicine (BUSM) have discovered a molecule that could help lead to the non-invasive detection of lung cancer as well as its treatment. Using RNA sequencing, the team looked at airway epithelial cells and identified a regulatory molecule that was less abundant in people with lung cancer and inhibits lung cancer cell growth. The findings, which are published in the Proceedings of the National Academy of Sciences, suggest that this molecule may aid in diagnosing lung cancer in earlier stages and could potentially, when at healthy levels, aid in treating the disease.
According to the National Cancer Institute (NCI), lung cancer is the leading cause of cancer death among both men and women in the United States, and 90 percent of lung cancer deaths among men and approximately 80 percent of lung cancer deaths among women are due to smoking. The NCI also estimates that approximately 373,489 Americans are living with lung cancer and its treatment costs approximately $10.3 billion in the United States each year.
MicroRNA’s are a new class of molecules classified as important regulators of the activity of other genes. In this study, the research team used a next-generation RNA sequencing technology and identified that a microRNA named miR-4423 in epithelial airway cells plays a major role in how these cells develop. In epithelial cells from the airway of smokers with lung cancer, levels of miR-4423 were decreased.
“These results suggest measuring the levels of microRNAs like miR-4423 in cells that line the airway could aid in lung cancer detection through a relatively non-invasive procedure,” said Avrum Spira, MD, MSc, the Alexander Graham Bell professor of medicine and chief of the division of computational biomedicine at BUSM, one of the study’s senior authors.
Using experimental models in vitro and in vivo, the research team demonstrated that miR-4423 can both promote the development of the normal airway cells and suppress lung cancer cell growth. This suggests that miR-4423 plays a major regulatory role in cell fate decisions made by airway epithelial cells during maturation and low levels of miR-4423 contributes to lung cancer development. Interestingly, throughout the body, miR-4423 seems only to be present in high levels in the airway epithelium, suggesting this could be a very specific process occurring only in the lungs.
“Our findings open up the option to study whether returning the levels of miR-4423 to normal in the airway could help stop cancer growth and potentially be a way to treat lung cancer,” said Catalina Perdomo, PhD, a researcher in the division of computational biomedicine at BUSM who is the paper’s lead author.
“Interestingly, when we examined the genomes of other species for microRNAs that might function like miR-4423, we did not find anything in non-primates,” said Marc Lenburg, PhD, an associate professor in computational medicine and bioinformatics at BUSM who is one the study’s senior authors. “It makes us wonder what it is different about lung development in primates and excited that this could be a very specific process to target for lung cancer treatment.”
This study was funded in part by the National Institutes of Health’s National Cancer Institute Early Detection Research Network under grant award numbers R01 CA 124640 and U01 CA152751; the National Science Foundation Integrative Graduate Education and Research Traineeship under grant award number P50CA58184; and Merit Review grants 5I01BX000359 and R43HL088807-01.
Journal Reference: Perdomo C, Campbell J.D., Gerrein J, Tellez C, Garrison C.B., Walser T.C., Drizik E, Si H, Gower A.C., Vick J, Anderlind C, Jackson G.R., Mankus C, Schembri F, O'Hara C, Gomperts B.N., Dubinett S.M., Hayden P, Belinsky S.A., Lenburg M.E., Spira A (2013) MicroRNA 4423 is a primate-specific regulator of airway epithelial cell differentiation and lung carcinogenesis. Proc Natl Acad Sci USA, 10.1073/pnas.1220319110 PMID: 24158479
Links to additional press: The Daily Free Press and Boston Magazine's HubHealth
Please click here to download editorial.