Deborah J. Stearns-Kurosawa, PhD
Associate Professor
Associate Provost/Dean ad interim for Graduate Medical Sciences
Contact Information
Email: dstearns@bu.edu
Research Interests
Why is it that some people get a bacterial infection, feel lousy for a few days, take antibiotics and then forget about it when they go back to class or work, but other people get the same infection and die in two weeks in the intensive care unit? It’s all about what pathogen is invading and how our bodies respond to the infection. It’s a highly orchestrated response that requires input from our immune, coagulation, neurologic, and inflammatory pathways. And this in turn requires coordinated responses from cells and molecules in each of these pathways. If the response is too much or inadequate, then disintegration can lead to multiple organ failure, shock and death. We have multiple NIH-funded projects to identify contributions at the host, organ, cellular, molecular and genetic level that contribute to different responses to infection. We want to identify the point where this disintegration process remains reversible, so that patients can be identified earlier with better prognosis and less morbidity. Current laboratory interests include:
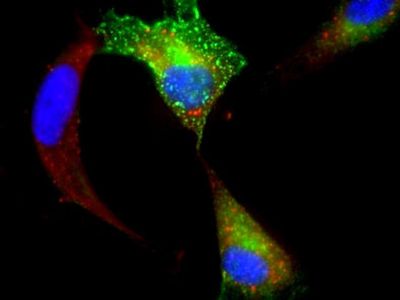
- Study of enteric Shiga toxin-producing E.coli (STEC) infection and the Shiga-like ribosome inactivating toxins from these bacteria. The prototypic strain is E.coli O157:H7, a persistent global public health problem. Antibiotics make the disease worse and STEC infection is the leading cause of acute kidney failure in young children in the US. We are developing clinically-relevant animal models to test therapeutics that work in the blood stream, in the intestinal tract and inside cells where the bacterial toxins invade (see Figure). Related projects include study of toxin distribution mechanisms in murine models, toxin-induced cellular stress responses, gene profiling of cellular responses to toxins, mathematical modeling of physiologic responses, and vaccine studies.
- Study of B.anthracis (anthrax) infection in a clinically relevant animal model. Our laboratory altered the anthrax disease paradigm by demonstrating the critical contribution of the host septic response to the lethality of anthrax infection and showed how adjunctive therapeutics can be beneficial. Model characterizations include physiology changes, metabolic indicators, biomarkers of coagulation, inflammation and innate immunity, and antigen-specific B cell responses after challenge with bacteria, toxins or spores. Therapeutics are studied at different disease stages and vaccine approaches are evaluated and validated in the primate models for application in both civilian and military populations.
- Study of how other pathologic conditions contribute to septic responses. One school of thought is that the decades of failed clinical trials to treat severely septic patients may be because research models have not taken into account co-morbidity contributions. Patients often are burdened with multiple problems, like obesity, diabetes and/or autoimmune disease, at the time they get a severe bacterial infection. Each of these health problems have their own set of contributions to the pathways that respond to bacterial infection, and very little is known about how networked responses are altered accordingly.
Representative Publications
- Stearns-Kurosawa, DJ, Osuchowski MF, Valentine C, Kurosawa S, Remick DG. The Pathogenesis of Sepsis. Annu Rev Pathol Mech Dis 6:19-48, 2011. Epub ahead of print 21Sept 2010 (PMID: 20887193).
- Stearns-Kurosawa, DJ, Collins V, Freeman S, Tesh VL, Kurosawa S. Distinct Physiologic and Inflammatory Responses Elicited in Baboons after Challenge with Shiga Toxin Type 1 or 2 from Enterohemorrhagic Escherichia coli. Infect Immun 78(6):2497-2504, 2010. (PMID: 20308301
- Kinasewitz G, Stearns-Kurosawa DJ, Kurosawa S. Soluble Thrombomodulin: a sign of bad times. Crit Care Med, 36(3):985-7, 2008. (PMID: 18431290
- Stearns-Kurosawa DJ, Lupu F, Taylor FB Jr, Kinasewitz G, Kurosawa S. Sepsis and pathophysiology of anthrax in a non-human primate model. Am J Pathol, 169:433-444, 2006 (PMID: 16877346).
- Kaneko T, Stearns-Kurosawa DJ, Taylor, Jr. F, Twigg M, Osaki K, Kinasewitz GT, Peer G, Kurosawa S. Down-modulation of neutrophil CD10 expression in non-human primates and humans after in vivo septic challenge. SHOCK 20:130-137, 2003 (PMID: 12865656).