More Than Just Skin Deep: BUSM Center Transforms Skin Cells into Stem Cells
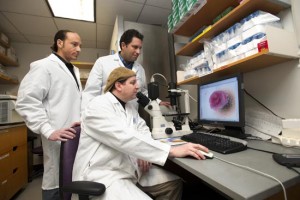
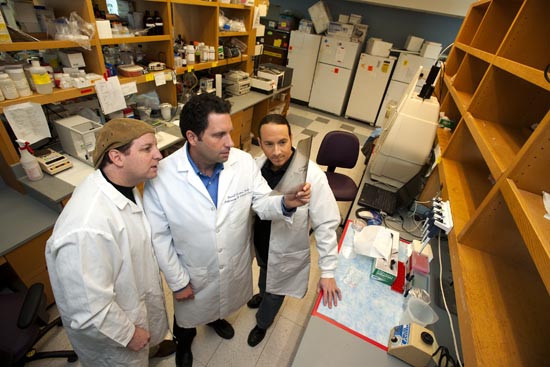
Darrell Kotton, Gustavo Mostoslavsky, and George Murphy roll up their sleeves and proudly display small oval marks on their forearms. Biopsies from which the medical researchers harvested their own skin cells to create—well, actually the sky may be the limit.
“Pretty much all the biology books are wrong now,” says Murphy, a School of Medicine assistant professor of medicine, who specializes in hematology. “Because they all say that your skin cells, your skin fibroblasts are always going to be fibroblasts. Turns out now they can become cells like an embryonic stem cell, which can then differentiate into any kind of cell it wants.”
Murphy is talking about human induced pluripotent stem cells, or iPSC, which form the core of the work at BU’s Center for Regenerative Medicine (CReM), a research facility he codirects with Kotton and Mostoslavsky that seeks to advance stem cell research. The collaborative effort among scientists on the Medical and Charles River campuses unites teams of stem cell biologists, physician-researchers, and biomedical engineers. CReM focuses on developing new treatments for diseases commonly seen at Boston Medical Center, such as cystic fibrosis, sickle cell anemia, emphysema, amyloidosis, and inflammatory bowel disease. The use of iPSCs, first developed in 2006 at the University of Kyoto, reduces dependence on the controversial, and federally limited, embryonic stem cell lines.
Last fall, the three CReM codirectors announced the creation of a bank of more than 100 lung disease–specific stem cell lines from patients with inherited diseases, including cystic fibrosis, alpha 1 antitrypsin deficiency emphysema, and sickle cell anemia. The lines mark the first time lung disease–specific iPSC have been created in a lab. The research was funded by the National Institutes of Health, the Cystic Fibrosis Foundation , and an ARC award from BU’s Evans Center for Interdisciplinary Research .
Led by pulmonary specialist Kotton, a BUSM associate professor of medicine, the team took tissue samples from patients with the diseases. Using a tool that Mostoslavsky, a BUSM assistant professor of medicine specializing in gastroenterology, engineered in 2008, called the stem cell cassette (STEMCCA), the team was able to reprogram adult skin cells into clinical-grade pluripotent stem cells. Mostoslavsky’s design, which BU has since patented, is now used by hundreds of labs around the world and is considered the industry standard.
“Our dream was to make a better tool, a viral vector to pop these genes into cells and do the equivalent of the University of Kyoto experiment that was better, safer, more efficient, and allowed translation to human beings in a way that was very simple and elegant,” Kotton says.
Many scientists believe that stem cells will play a crucial part in the fight against Parkinson’s, Alzheimer’s, and a range of genetic diseases, but in the United States, because of the use of human embryos, government injunctions against their use have been issued and lifted and issued again. Even with the high-quality iPSC lines CReM has developed, embryonic stem cells are still necessary to serve as a positive control: “a roadmap for developmental biology,” as Kotton puts it.
“Using induced pluripotent stem cells removes the necessity of using a human embryo and thus avoids all of the ethical problems of egg donation, embryo creation, and embryo destruction for research purposes,” says George Annas, William Fairfield Warren Distinguished Professor and chair of the School of Public Health health law, bioethics, and human rights department. “The primary scientific research issue is determining whether or not iPSCs are as pluripotent as human embryonic stem cells, and whether they are as predictable and abnormality-free from a genetic and epigenetic standpoint.”
From lab to bedside
Murphy often uses a “flight recorder” analogy when he explains his work.
“When there’s a plane crash, investigators look for the flight recorder so they can determine each event that led up to the catastrophic event,” he says. “In much the same way, we can take skin cells from sick patients and differentiate those cells into the affected tissue type and go through all the molecular events that led up to the disease and that catastrophic event. It creates the ability to intervene early.”
Human induced pluripotent cells also allow drug developers and scientists more precision, offering a quality even embryonic cells don’t offer. The use of a person’s own skin or blood to create embryonic-like stem cells means the patient’s body won’t reject them, thereby eliminating the need for immunosuppressive drugs.
“You’re looking at cells and the disease in the context of the exact genetic background of that patient,” Murphy says. “So it becomes possible to test therapeutic drugs in the test tube before using them on patients. It’s patient-specific medicine.”
A seminal CReM project, which got under way in 2009, involves an infant in New York City with inherited long QT syndrome, which causes a serious heart arrhythmia. Kotton and his team took skin cells from the baby, as well as from the parents, and generated iPSC, which in turn were programmed to differentiate into heart muscle cells, or cardiomyocytes. CReM researchers are coordinating with laboratories in New York and Toronto to test available pharmaceuticals on those cardiomyocytes, which in essence act as the disease in miniature, to determine how best to treat the sick child.
The team has also collaborated with researchers at Massachusetts General Hospital to engineer a bioartificial rat lung that allowed a living rat to breathe for six hours. Further, they’ve developed a gene therapy that offers lifetime protection against an inherited form of emphysema in mice.
Fast friends
The three researchers have a tight bond and play well off each other. They first met as postdocs in the lab of prominent stem cell biologist Richard Mulligan at Harvard Medical School. They became fast friends and fit together like puzzle pieces.
“Darrell’s the mature statesman, Gustavo’s the passionate Argentinian, and I’m the crazy adolescent,” says the 37-year-old Murphy, who sports a ponytail and an earring in each ear.
Kotton first arrived on campus as a fellow in pulmonary and critical care medicine in 1998, and after his subsequent postdoctoral research fellowship at Harvard, he returned to MED in 2004, starting his own lab focusing on lung stem cell work. In 2008, Mostoslavsky was recruited, followed soon after by Murphy.
“Like many centers, ours is formed on scientific passion, but it’s also formed on a deep friendship that came before the center,” Kotton says. “Our main interest is love of science. We’re in love with the cells and what controls their cell fate decisions and their biology, and a wonderful side effect of all these projects is they may end up helping people, which is a great thing.”
This BU Today story was written by Caleb Daniloff. He can be reached at cdanilof@bu.edu.