Post-Overdose Outreach Before and After COVID

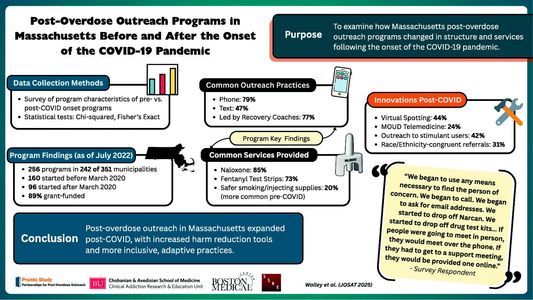
Several research faculty and staff in the Section of General Internal Medicine (GIM) surveyed Massachusetts post-overdose programs about their practices before and after the onset of the COVID-19 pandemic. In collaboration with colleagues at the Boston University School of Public Health, St. George’s University, and Social Science Research and Evaluation Inc., GIM faculty and staff on the PRONTO team asked post-overdose programs about programming onset, funding, outreach encounters, naloxone distribution, medication for opioid use disorder (MOUD) referrals, and program practices before and after the pandemic. They published their findings in an article titled “Post-overdose outreach programs in Massachusetts before and after the onset of the COVID-19 pandemic” in the Journal of Substance Use & Addiction Treatment.
As stated in the publication abstract, the team identified 256 programs active in 69% of Massachusetts’ 351 municipalities. “Before March 2020, 160 ‘pre-pandemic onset’ programs were active. After March 2020, 96 ‘post-pandemic onset’ programs started. In 2022, most were grant-funded (89% (227/256)). Initial survivor contact was attempted via phone (79% (201/256)) and text (47% (120/256)), most commonly by a recovery coach (77% (196/256)). Most programs offered fentanyl test strips and naloxone. Some programs, more commonly pre-pandemic onset, offered safer smoking and injecting supplies. Among the 160 pre-pandemic onset programs, new practices included recommending virtual spotting (44 % (70/160)), facilitating MOUD telemedicine (24 % (39/160)), outreach for people using cocaine and methamphetamine (42 % (67/160)), and referring to race and ethnicity congruent services (31 % (50/160)).”’
The study concluded, “Massachusetts post-overdose outreach programs expanded following the COVID-19 pandemic onset. Services and innovations included resources to reduce harms from the unregulated drug supply (e.g., fentanyl test strips) and more inclusive outreach (e.g., include people using stimulants and race and ethnicity congruent services).” Their findings demonstrated that these programs were able to sustain themselves and adapt with the onset of the COVID-19 pandemic. The publication also noted, “Reducing the risk of future overdose among overdose survivors was the highest-ranked goal among both pre- and post-pandemic programs.” The authors add, “In the post-pandemic onset context, the next steps include understanding how programs can continue engaging overdose survivors and their families in harm reduction, treatment, recovery support, and social services in the midst of a changing drug supply.”