Gates Grant in Hand, BUSPH Researcher Prepares to Fight Newborn Mortality in Zambia
As an infectious disease specialist, Dr. David Hamer, an associate professor of international health at the BU School of Public Health, deals in people, not percentages.

Still, when it comes to child mortality, the numbers weigh on Hamer’s mind.
In the plus column, the number of children who die before their fifth birthdays each year has fallen below nine million for the first time on record, a significant milestone in the global effort to improve children’s chances of survival. In the minus column, the proportion of those under-five deaths occurring in the first 28 days of life has climbed to 40 percent, with three-quarters of those deaths occurring in the first week of life, indicating that more needs to be done to save newborns in their earliest days.
That’s where Hamer will spend the next four years focusing his attention. He will lead a team of researchers from BU’s Center for Global Health and Development (CGHD), based at the BU School of Public Health, in testing whether a low-cost antiseptic wash can reduce infections of the umbilicus in the month after birth and prevent the deaths of newborns from those infections. The large-scale trial, which will be undertaken in the African nation of Zambia, is funded by an $8.4 million grant from the Bill & Melinda Gates Foundation.
Hamer will work with BUSPH researchers Katherine Semrau, Kojo Yeboah-Antwi, and Julie Herlihy. CGHD Director Jonathon Simon and International Health Professor Donald Thea will oversee the study.
Hamer recently spoke about the project and other work to reduce neonatal mortality:
Q: Why has there been so much progress in reducing under-five mortality, but not much progress in reducing neonatal deaths — those in the first four weeks of life?
A: In the last 10 to 15 years, there’s been a major push to reduce child mortality, to meet the U.N. Millennium Development Goal of a two-thirds reduction in under-five mortality by 2015. Some countries have made significant progress and will make that target; others probably won’t. The major focus so far has been on addressing malaria, nutrition, pneumonia and diarrhea in those early years, which has helped to reduce those under-five deaths. But the causes of neonatal mortality are different. When we look at the first month of life, we’re talking about other factors: prematurity, birth asphyxia, sepsis and hypothermia. They require different kinds of interventions.
Q: Has there been any notable progress in interventions targeted to those neonates?
A: Some, yes — and we [at Center for Global Health and Development] have had a hand in that.
Most of the research to date has been based in South Asia – India, Nepal, Bangladesh, Pakistan – with relatively little being done in sub-Saharan Africa, which has very different ecological and socio-cultural challenges. The population in Africa is much more spread out, and there are major human resource deficits, in terms of not enough health facilities, not enough doctors. So what we’ve increasingly recognized is that we need to provide community-based care, through cadres of community health workers, in the absence of an institutional infrastructure. That means task-shifting.
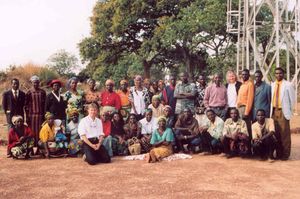
We did that successfully with a project we undertook in Zambia called LUNESP, where we trained traditional birth attendants in the Lufwanyama district in some simple interventions to prevent hypothermia, sepsis and asphyxia in the first 28 days of life. We had some very promising results, in terms of reducing mortality. Now we’re working with Save the Children and USAID to continue that program and eventually scale it up to include community-based treatment of pneumonia, diarrhea treatment with zinc, and also to integrate community health workers into managing the infant’s health within that first month of life.
Q: Isn’t the first step in tackling neonatal mortality to make sure that healthcare workers can identify an unhealthy vs. healthy baby?
A: Absolutely, that’s the first challenge. And actually, one of the studies I was involved in — conducted by the Young Infants Clinical Signs Study Group and published in The Lancet in 2008 — looked at that issue. We looked at infants under two months old who were brought to health facilities in six countries, and we assessed their symptoms and clinical signs of illness. We were able to come up with seven sets of symptoms that predicted severe illness — things like difficulty feeding, high respiratory rate, severe chest in-drawing, high temperature — in order to give first-level healthcare workers a kind of checklist to identify infants who needed referral for potentially life-threatening illnesses. Those guidelines went to the World Health Organization and became official health policy, and were also adopted by individual countries. That was exciting.
Q: How did this new Gates grant for the umbilical cord washing project come about?
A: I was at a meeting last year, actually, and ended up talking to a representative from the Gates Foundation about our interest in neonates. The Gates Foundation is focusing on the continuum of care from the mother’s health, through the early postnatal period, through childhood, and they recognize the need for interventions that can be carried out in a community setting. They were aware of our success with the LUNESP project, which was aligned with that strategy. So we were really on the same page, when it came to this new intervention — training healthcare workers and mothers to use chlorhexidine [an antiseptic wash] to clean the umbilicus stump of newborns.
Q: How big an undertaking is the new study?
A: It’s huge. We will enroll deliveries at 90 health facilities in southern Zambia and hire a team of about 150 people, many of them data collectors who will help us track what happens to these babies. Half of the neonates will have dry cord care — a soap and water wash right after the cord is cut — which is the standard practice in Zambia now and is recommended by the WHO. With the other half, healthcare workers, traditional birth attendants and family members will apply chlorhexidine, which has been found to reduce infection rates. There’s been only one published study on chlorhexidine and cord care, in Nepal, and it found that if chlorhexidine is applied in the first 24 hours, the risk of death is significantly reduced, by close to 35 percent. So that’s a positive sign.
There’ll be a companion study done in Pemba Island, Zanzibar, by a team from Johns Hopkins. So by the time we’re done, we’ll have a lot of data. The hope is, if all the studies show that chlorhexidine has an impact on neonatal mortality, we’ll be able to make the case that global policy needs to change. That’s an exciting possibility.
Submitted by Lisa Chedekel