A COVID-19 Primer for the Boston University Community
Based on resources from US Centers for Disease Control and Prevention, World Health Organization, Massachusetts Department of Public Health and others. Compiled by Nahid Bhadelia, MD, MA, Associate Professor, Medicine/Infectious Diseases, and Ronald Corley, PhD, Professor of Microbiology and Director, National Emerging Infectious Diseases Laboratories.
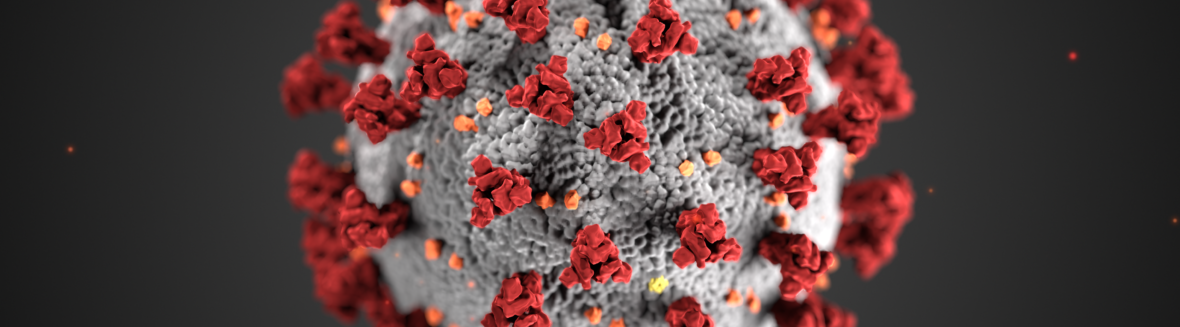
What is COVID-19?
COVID-19 is a flu like illness that’s caused by SARS-CoV-2. Large case series (majority of them from China) show that around 80-85% of people who are infected have just mild illness with cough and fever, while a smaller percentage (generally those who are older or may have other comorbidities) around 14% can have a more severe disease with presentation of pneumonia and requiring hospitalization. A smaller percentage still (around 5%) may become critically ill. Of people who are symptomatic, the case fatality rate is around 2.3%.
Here are some informative factsheets:
CDC: https://www.cdc.gov/coronavirus/2019-ncov/downloads/2019-ncov-factsheet.pdf
WHO: https://www.who.int/health-topics/coronavirus
NIAID: https://www.niaid.nih.gov/diseases-conditions/coronaviruses
Here is a link to one of the largest case series published to date: https://jamanetwork.com/journals/jama/fullarticle/2762130
There may be other patients who are infected with this virus who do not have any symptoms. We currently do not know how many people fall into this group.
Where did SARS-CoV2 come from?
Per CDC, “The SARS-CoV-2 virus is a betacoronavirus, like MERS-CoV and SARS-CoV. All three of these viruses have their origins in bats. The sequences from U.S. patients are similar to the one that China initially posted, suggesting a likely single, recent emergence of this virus from an animal reservoir.”
Most experts agree the current SARS-CoV-2 also most likely originated from bats and at some point “spilled over” into the human population, perhaps via an intermediate mammalian host.
How is it transmitted?
The virus can spread mainly from person-to-person through close contact (within about 6 feet) and through respiratory droplets produced when an infected person coughs or sneezes.
These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. It can also be transmitted to a lesser extent if a person touches a surface or object that has the virus on it and then touches their own mouth, nose, or possibly their eyes. Although people are most likely to transmit the virus to others when they are sick, there have been reports that this virus could be transmitted before a person manifests symptoms. The frequency of how often the latter happens is not known. There is also evidence that people may still shed some virus after they recover from the disease (as is noted in influenza and other respiratory virus).
How does this virus compare to the seasonal flu? Updated
Although both cause similar symptoms, SARS-CoV-2 is thought to be less transmissible than seasonal influenza but have a higher mortality rate.
The other aspects of SARS-CoV-2 that are difficult are that we current do not have a vaccine like we do for seasonal influenza and we are still learning about the disease.
How long does it take to get sick if you are exposed (what is the incubation period)?
Symptoms usually appear within 3-7 days, but current estimates by CDC is that the latency period is as few as 2 to as many as 14 days on average. There are a few reports of longer incubation periods.
What are the symptoms?
In a report by WHO about the cases in china- the following symptoms were reported with decreasing frequency were as follows: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), muscle or bone pains (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%). In most cases, patients will present with a fever and cough.
How widespread is COVID-19?
As of Feb 29, 2020, more than 86,000 patients have been diagnosed with COVID-19 worldwide, of which around 3,000 have died.
Per CDC, On Jan. 30, 2020, the International Health Regulations Emergency Committee of the World Health Organization declared the outbreak a “public health emergency of international concern ” (PHEIC). On Jan. 31, 2020, Health and Human Services Secretary Alex M. Azar II declared a public health emergency (PHE) for the United States to aid the nation’s healthcare community in responding to COVID-19.
While majority of the cases to date have been in China, COVID-19 has been reported in 64 countries and territories as of Feb 29. Because of the spread of COVID-19 into an increasing number of countries, on Feb 28, 2020, the WHO increased the risk assessment to a “very high at a global level”.
This frequently updated website offered by Johns Hopkins University offers more details regarding the breakdown of cases; https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
Other resources include the WHO (https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd)
As well as live updates on “worldometer” (https://www.worldometers.info/coronavirus/)
In United States, as of Feb. 29, there are currently 68 confirmed cases of COVID-19, which are a mix of people who are returning travelers, citizens repatriated from the Diamond Princess cruise ship in Japan and those who were infected on U.S. soil.
How are people who may potentially have COVID-19 identified?
Currently, when patients present with symptoms which appear to be similar to COVID-19 and have a travel history to one of the areas where a large number of cases have been identified or have had exposure to someone with confirmed COVID-19, or if they present with severe illness with no other explanations, they are identified by medical providers as fitting the “case definition” for COVID-19 as set by the CDC. The current case definitions from the CDC can be found: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html
At that point, samples are collected from the patients and sent to one of the laboratories with the capacity to test for SARS-CoV-2. The current diagnostic procedure involves a polymerase chain reaction (PCR) detection of the SARS-CoV-2 virus in nasopharyngeal and oropharyngeal swabs.
Are there vaccines or treatments for it?
There are currently no vaccines or targeted treatments for COVID-19, however both are currently in the process of being developed. Clinical trials will begin on at least one therapeutic (Remdisivir, from Gilead Sciences) and the NIH is beginning a clinical trial of a vaccine candidate from Moderna, Inc., a biotechnology company based in Cambridge, Mass.
There are currently no post exposure prophylaxis treatments available to give to those exposed to the disease either.
Will COVID-19 spread further in the United States?
There is a growing number of cases identified as those from community transmission- this means that these patients didn’t have any known exposures to someone with COVID-19 or travel history that would put them at risk. Public health officials have reported that it is likely that we will see more cases of COVID-19 and potentially a bigger epidemic in the United States.
What will happen if there is more spread of COVID-19 in United States?
Given what we know about COVID-19, most people who get the disease will have a very mild illness. However, a smaller percentage (currently thought to be around 15%) of people, particularly those over the age of 60 and/or with other medical conditions may get more severe infection that requires hospitalization.
Current recommendations from the CDC are that people who are sick do not go into work (voluntary isolation).
If there is sustained transmission of COVID-19 in certain areas of the United States, public health officials may call for cancellation of large events (such as large conferences, concerts, sporting events etc) to keep people from transmitting to each other. Additionally, as seen in other countries, public health officials may suggest that schools be closed for a limited period of time and people work from home. However, the exact measures will depend on how big an epidemic we see in the United States.
How are healthcare facilities preparing for potential spread of COVID-19 in United States?
Healthcare facilities are working to strengthen existing systems and put new systems into place to quickly identify patients with symptoms and travel history, encouraging those who are not very sick to stay home and call their providers for advice, retraining healthcare workers, ensuring there are enough supplies of personal protective equipment.
How should I protect myself from becoming infected?
First and foremost, because of the way this virus is transmitted, CDC recommends:
- Voluntary Home Isolation: Stay home when you are sick with respiratory disease symptoms. At the present time, these symptoms are more likely due to influenza or other respiratory viruses than to COVID-19-related virus.
- Respiratory Etiquette: Cover coughs and sneezes with a tissue, then throw it in the trash can.
- Hand Hygiene: Wash hands often with soap and water for at least 20 seconds; especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.
- If soap and water are not readily available, use an alcohol-based hand sanitizer with 60%-95% alcohol.
- Environmental Health Action: Routinely clean frequently touched surfaces and objects
The reasons masks don’t generally protect health people against respiratory viruses are because they are generally not used accurately by those without training (people can still become infected if their hands are contaminated and their touch their nose, mouth and eyes); lead to false sense of security which makes people not pursue appropriate social distancing that would be more effective; and masks become quickly wet and then ineffective as a barrier. On the other hand, given the shortages in masks and other protective equipment, such widespread use by public is reducing availability of masks for healthcare workers and those who actually have the symptoms who can use the mask to reduce transmission to those around them.
The most effective strategy is hence – if you are well – keep a distance from those who have respiratory symptoms; make sure you frequently wash your hands or sanitize them; and reduce the frequency with which you touch your face with your hands.
How should I prepare myself and my family for COVID-19?
Currently, you can prepare by reading these excellent guides from CDC and WHO:
https://www.cdc.gov/coronavirus/2019-ncov/preparing-individuals-communities.html
https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/guidance-for-schools.html
https://www.cdc.gov/coronavirus/2019-ncov/downloads/2019-ncov-factsheet.pdf
WHO: https://www.who.int/docs/default-source/coronaviruse/getting-workplace-ready-for-covid-19.pdf
Make sure you have tools to sanitize and wash your hands and decontaminate your environment. You could also consider buying a small supply of cold and fever medications if you don’t already have them in your house, so if you get sick you do not have to go to the pharmacy. If you are on prescription medications, make sure you refill your medications, so you have them at hand. If your insurance allows it, consider seeing if your mail in pharmacy could send you a multiple month supply of your prescriptions.
It may be good to keep some extra dry foods, ready-to-eat meals and soups around the house so that if you become sick you do not have to venture to the grocery stores.
If you are a caretaker for elderly person or someone with multiple comorbidities, ensure that you help them with some of the preparedness in their homes.
What should I do if I think I have COVID-19?
The guidance from CDC is to stay home except to get medical care, separate yourself from other people and animals as much as possible. If possible, stay in a separate room and use a separate bathroom. Before going to a health care provider, call ahead to reduce the risk of exposing others to the virus. Cover your coughs and sneezes, wash your hands often, and clean surfaces you frequently come into contact with. Monitor you symptoms, and call your healthcare provider is you get worse. Additional information can be found at:
https://www.cdc.gov/coronavirus/2019-ncov/about/steps-when-sick.html
What will happen if someone in the BU community develops COVID-19?
BU will follow guidance from Boston Public Health Commission, the Massachusetts Department of Public Health and the CDC.
In the City of Boston, the Boston Public Health Commission is responsible for responding to public health threats, such as COVID-19. Their most recent advisory can be found at:
What is BU doing to protect its staff, faculty and students?
Depending on your work space, you should have access to occupational health or student health resources. Make sure you have their number ready if you feel sick to receive guidance. Please call rather than go to occupational health offices as you may be advised to go home based on guidance from BPHC.
BUSPH is sponsoring a panel on COVID-19 on March 12: https://www.bu.edu/sph/news-events/signature-programs/deans-seminars/deans-seminar-series-on-contemporary-issues-in-public-health/coronavirus-what-do-we-know-what-do-we-not-know-what-should-we-be-doing/
Additionally, the University will share timely information with its community about school closures if so indicated by public health officials.
What can I do to reduce chances of transmitting this disease?
Aside from ensuring that you perform good hand washing and sanitizing practices as well as covering you nose and mouth with your elbow if you are coughing or sneezing (respiratory etiquette), you should stay home when if you are sick.
The CDC recommends the following:
Personal Protective Measures. During an outbreak in your community, CDC recommends the everyday preventive measures listed above—especially staying home when sick—and taking these additional measures:
- Keeping away from others who are sick.
- Limiting face-to-face contact with others as much as possible
- Consulting with your healthcare provider if you or your household members are at high risk for COVID-19 complications
- Wearing a facemask if advised to do so by your healthcare provider or by a public health official
- Staying home when a household member is sick with respiratory disease symptoms, if instructed to do so by public health officials or a health care provider (Voluntary Home Quarantine)
Community Measures. If COVID-19 disease is occurring in your community, state and local public health authorities may decide to implement:
- Temporary closures or dismissals of childcare facilities and schools
- Other social distancing measures that increase the physical space between people, including:
- Workplace social distancing measures, such as replacing in-person meetings with teleworking
- Modifying, postponing, or cancelling mass gatherings.
Decisions about the implementation of community measures will be made by local and state officials, in consultation with federal officials as appropriate, and based on the scope of the outbreak and the severity of illness. Implementation will require extensive community engagement and ongoing and transparent public health communications.
https://www.cdc.gov/coronavirus/2019-ncov/preparing-individuals-communities.html