How Virtual Reality Might Help Fight Recurring Nightmares
BU researchers: VR could benefit people, particularly children, suffering scary dreams

You might say that Patrick McNamara is in a frightening line of work. As a sleep researcher, he’s hunting for new ways to treat people with nightmare disorder (also known as dream anxiety disorder). Being chased by a malevolent entity, McNamara says, is one of the most common recurring nightmares that patients report experiencing over and over again.
“Very often, people with chronic nightmares report dreaming about being chased or attacked by supernatural or demonic beings,” says McNamara, a Boston University School of Medicine associate professor of neurology. “They can’t really see their attackers’ faces, but they know their intent is to harm them. People also report being chased by animals like snakes or bears. Bears are very frequent in these types of dreams, where you’re trying to get safe, throwing up obstacles between you and the attacker, feeling like you’re about to be attacked.”
A nightmare like that might give anyone a bit of anxiety. But terrifying dreams, if they keep happening, can induce far more than just fleeting fear. McNamara says recurring nightmares can have profound long-term effects, especially for children who experience them. In the United States, between half and two-thirds of children and up to 15 percent of adults have frequent nightmares.
“Recurring nightmares are really significant predictors,” he says. “They foretell mental health trouble.”
For children, that trouble can come in the form of adolescent and adult psychosis, including anxiety, depression, stress, and suicidal ideation. In adults, distressing nightmares can often be a sign of post-traumatic stress disorder (PTSD). Despite the documented clinical effects of nightmares—including distress, loss of sleep, and generalized anxiety—McNamara says we still lack easy-to-use, effective treatments for nightmare disorders.
Imagery rehearsal therapy, the current gold standard for treatment, attempts to teach patients to replace nightmare imagery with less frightening versions. According to McNamara, the success of the treatment is varied and typically short-term because it relies on a person’s ability and willingness to conjure up realistic nightmare imagery in their mind’s eye, which some patients can do better than others. Naturally, most young children are even less capable of willfully controlling an imagined visual narrative than adolescents or adults.
How can you stop recurring nightmares?
Research in the last decade has hinted that modern technology may enable a more tangible approach to treating nightmare disorders. In 2010, Grant MacEwan University psychologist Jayne Gackenbach found that people who played video games before bed may have better awareness and control in their dreams, which could help prevent distressing nightmares. Then, in 2011, Gackenbach found that soldiers who played warfare-themed video games were less likely than nongamers to suffer from feeling distress and helplessness in their dreams.
The takeaway from those studies? Platforms like video games that exercise a person’s ability to control and manipulate simulated imagery—rather than imagery conjured up in their mind’s eye—could have therapeutic benefits for people with nightmare disorders. Looking out to the next evolution of visual technology, McNamara became very interested in whether virtual reality could be an even more effective tool.
“Virtual reality immerses you in a 3-D environment and the imagery is quite intense,” McNamara says. How intense? The sensory inputs can be so all-consuming that “even for people who do it often, you can get nausea because it destabilizes the inner brain mechanisms about balance.”
Virtual reality programs place users into artificial environments where they experience and manipulate visuals that seemingly exist right in front of their own eyes. In this way, McNamara says, VR is able to take the burden of imagery generation off of the patient, immersing them in nightmarish imagery through interactive systems like Oculus Rift.
The hardest thing to grasp is the idea that recurring nightmares never lose their strength. It’s a really painful problem to have nightmares that are just as bad the hundredth time you’ve had them.”—Wesley J. Wildman
Teaming up with Wesley J. Wildman, a BU School of Theology professor of philosophy of religion and an expert in artificial, computer-simulated environments, McNamara designed a pilot study to examine if virtual reality therapy could help people with recurring nightmares. The two are cofounding directors of the Center for Mind and Culture and have previously worked together to explore how religious experiences are processed in the brain.
When McNamara reached out to Wildman for help with the virtual reality component of the study, Wildman says, the idea struck him as a “genius-level intervention.”
For people who don’t experience recurring nightmares, “the hardest thing to grasp is the idea that recurring nightmares never lose their strength,” he says. “It’s a really painful problem to have nightmares that are just as bad the hundredth time you’ve had them.”
Ultimately, Wildman says, unrelenting nightmares can make people truly afraid to go to sleep.
Teaching control over dream imagery
For the pilot study, McNamara and Wildman designed moderately frightening virtual reality imagery—such as an underwater environment where a great white shark seems to swim closer and closer to the virtual reality user—to illicit a manageable level of fear in participants. “To treat nightmare disorders, you want to expose the person to arousing and disturbing images, but you don’t want to expose them to very scary images,” McNamara says. The goal is to treat distress rather than inflict more.
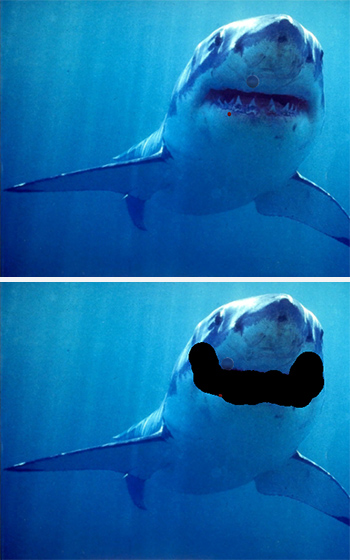
They enrolled 19 study participants who reported having frequent nightmares. Using joystick and gesture controls, participants were able to modify the threatening visuals to make them less scary. McNamara says they could, for example, use a drawing tool to cover up the shark’s teeth or a sizing tool to shrink it down. Afterward, participants were also asked to write a narrative about their newly edited visual experience.
Someone might say, “When I looked [at the shark] more closely it turned out to be a great white tuna that was going to swim by me,” McNamara says. “Suddenly that tremendous force is not after you and it’s not so threatening.”
Over the course of a month, participants continued visiting McNamara’s lab twice a week to use an Oculus headset and its joystick controls to alter scary visuals and create new narratives. Each visit, they were monitored for anxiety, nightmare distress, and nightmare effects. By the conclusion of the study, participants reported significantly lower levels of all three. The results were published in the journal Dreaming.
“We think that they learn these imagery control skills and then over a couple of weeks, those skills get transferred from their conscious state into their dream state,” McNamara says.
Although the results of the pilot are exciting, McNamara says the next step is to design a double-blind clinical trial to really test the effects of virtual reality therapy. To rule out placebo therapy effects, he says, such a study could involve a group of participants who do virtual reality therapy and another group of participants who do standard imagery rehearsal therapy.
“The most exciting thing about this is the potential to bring this to kids suffering from nightmares,” says McNamara. “Kids are fantastic with adopting technology, and if we can treat their nightmares earlier, we might slow down or prevent conversion into psychosis. That could save lives.”
The pilot project was funded by the Center for Mind and Culture and the Virginia Modeling, Analysis & Simulation Center.
This BU Today Story was written by Kat McAlpine.