The Management of Chronic Eosinophilic Pneumonia with Mepolizumab
Romy Lawrence, MD
Romy Lawrence MBBCH1, Elizabeth S. Klings MD1,2
1Department of Medicine, 2The Pulmonary Center, Boston University School of Medicine, Boston, MA
Introduction: Chronic eosinophilic pneumonia (CEP), an idiopathic inflammatory disorder characterized by the accumulation of eosinophils in the pulmonary interstitium and alveolar spaces, clinically presents with progressive dyspnea, productive cough and fever. The first line therapy for CEP is long-term corticosteroids which is effective in the majority of cases. However, 50-80% of patients relapse with corticosteroid cessation or tapering. Given the high rates of relapse and the significant toxicities associated with long-term corticosteroid use, alternative agents need to be explored. We present a patient with CEP requiring a prolonged course of prednisone with associated toxicity who was effectively treated with mepolizumab.
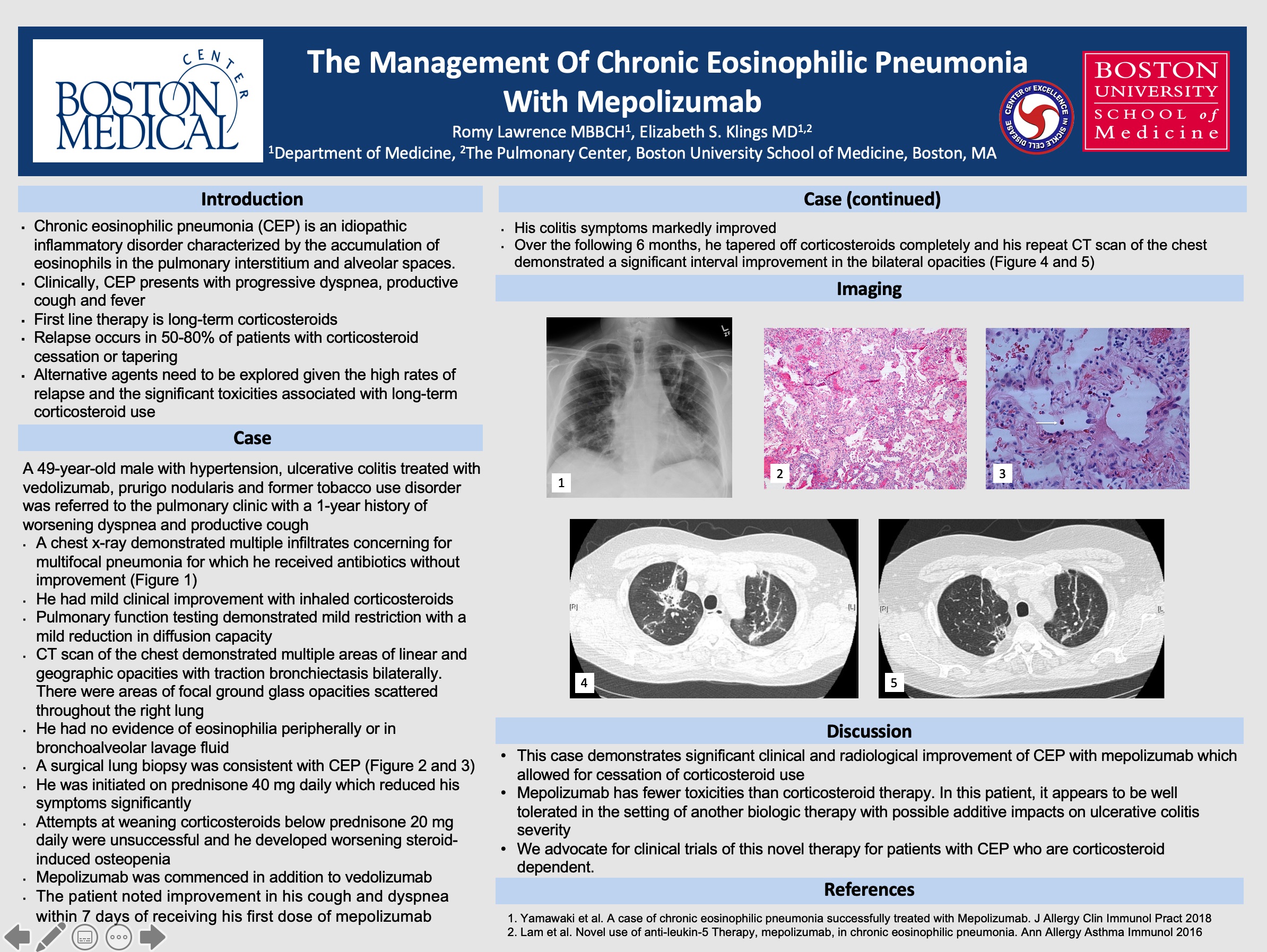
Case: A 49-year-old male with hypertension, ulcerative colitis treated with vedolizumab, prurigo nodularis and former tobacco use disorder was referred to the pulmonary clinic with a 1-year history of worsening dyspnea and productive cough. He had a chest x-ray concerning for multifocal pneumonia for which he received antibiotics without improvement. He noted some improvement with inhaled corticosteroids. Pulmonary function testing demonstrated mild restriction with a mild reduction in diffusion capacity. CT scan of the chest demonstrated multiple areas of linear and geographic opacities with traction bronchiectasis bilaterally and areas of focal ground glass opacities scattered throughout the right lung. His laboratory studies and a bronchoalveolar lavage (BAL) were unrevealing. He had neither a peripheral or BAL eosinophilia. A surgical lung biopsy was consistent with CEP. He was initiated on prednisone 40 mg daily which reduced his symptoms significantly. Attempts at weaning corticocsteroids below prednisone 20 mg daily were unsuccessful and he developed worsening symptoms related to osteopenia. After discussion with his gastroenterologist, it was decided to initiate mepolizumab in addition to vedolizumab. The patient noted improvement in both his cough and dyspnea as well as his colitis symptoms within 7 days of receiving his first dose of mepolizumab. Over the following 6 months, he tapered off corticosteroids completely and his repeat CT scan of the chest showed a significant interval improvement in opacities bilaterally (Figure 1).
Discussion:
This case demonstrates significant clinical and radiological improvement of CEP with mepolizumab which allowed for sparing of corticosteroid use. Mepolizumab has fewer toxicities than corticosteroid therapy and in this patient, appears to be well tolerated in the setting of another biologic therapy with possible additive impacts on ulcerative colitis severity. We advocate for clinical trials of this novel therapy for patients with CEP who are unable to be weaned off corticosteroids.
5 comments
Interesting case.
Romy, terrific example of using a case report to stimulate further studies. Great work! Dave
nice work – good to publish these clinical observations to stimulate the field!
Great case. what dose of Mepolizumab was used and what frequency?Thanks
How would you explain the lack of bal eosinophils in CEP?