End-of-Life Care in the ICU: Exploring Disparities in Timely Goals of Care Discussions
Stephen Russell, MD
Rationale
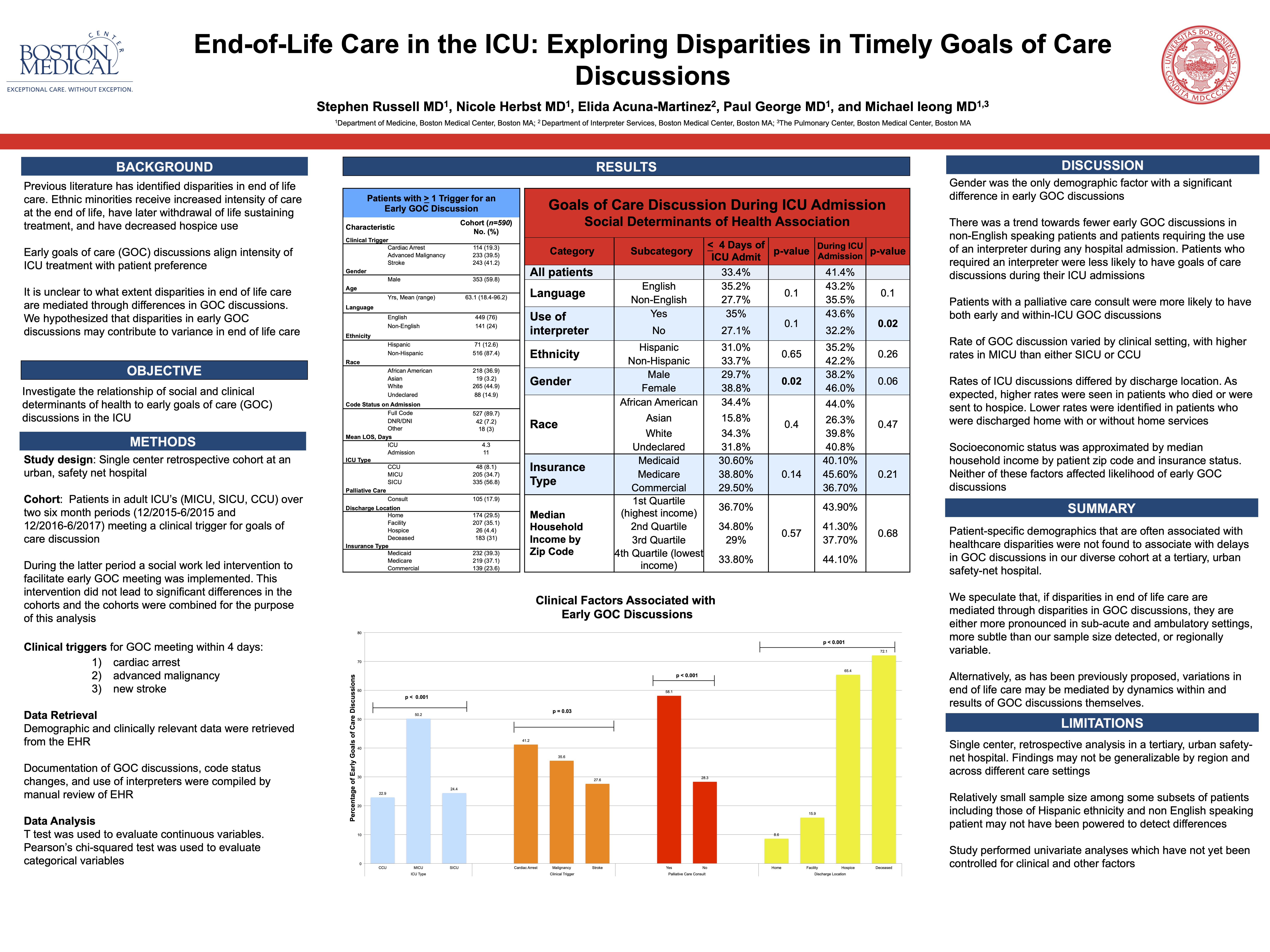
There is evidence for racial and ethnic disparities in the quality of end-of-life care discussions in the intensive care unit (ICU); however, less is known about whether differences exist in timing of these conversations. Goals of care (GOC) discussions with patients and families are key to providing appropriate, patient centered care. We hypothesized that patient factors including race/ethnicity, primary language, and socioeconomic status may affect the likelihood of timely GOC discussions in the ICU of an urban safety-net hospital.
Methods
We conducted a single center retrospective cohort study of patients with conditions associated with high short-term mortality that were admitted to the medical or surgical ICU of an urban, safety-net hospital. Patients were deemed likely to benefit from early GOC discussions based on the clinical triggers of stroke, cardiac arrest, or advanced malignancy. Data were collected over two six month periods between 2015 and 2017. During the later period, an intervention was implemented utilizing social workers to identify patients with a clinical trigger and facilitate an early GOC meeting. An early GOC meeting was defined as a chart documented family meeting occurring within 4 days of admission to the ICU. Interpreter data and palliative care data were provided by the respective departments. Self reported demographic data was obtained from the electronic health record and socioeconomic data by zip code was collected from publically available sources.
Results
We identified 601 patients meeting the eligibility criteria. Patients were more likely to have received an early GOC discussion in the medical ICU compared with the surgical ICU (62.3 vs 28.6%, p<0.001). Patients who were seen by the palliative care consult team were more likely to have had an early GOC discussion (65.7% vs. 36.3%, p<0.001). Other factors associated with early GOC were male gender (p=0.04) and disease severity (p<0.001). Patient characteristics not associated included race, ethnicity, age, language, need for interpreter during admission, insurance type, and median household income by zip code.
Conclusions
Patient-specific demographics that are often associated with healthcare disparities were not found to associate with delays in GOC discussions in our cohort. The likelihood of an early GOC discussion was affected by ICU setting, male gender, disease severity, and palliative care consultation. Strategies to anticipate and compensate for these differences may improve timeliness of a GOC meeting.
3 comments
Stephen, really interesting study! I’m relieved to see that race and ethnicity were not associated with different GOC rates. Well-done! Dave
Really happy to see that your early interest in this topic (which I remember from advising days) has led to this important work.
nice job on an important topic in end of life care!