Researchers Discover a New Beneficial Function of an Ancient Protein
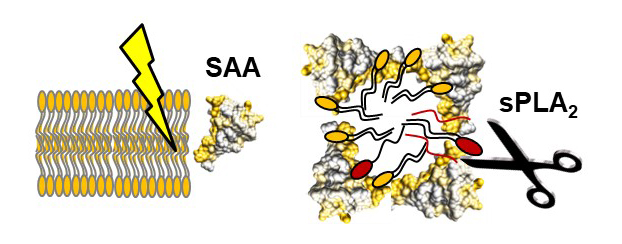
Cell boundaries are made of lipids. When cells are severely damaged, these lipids need to be rapidly removed to avoid toxicity and facilitate tissue healing. Researchers have discovered that a small ancient protein, Serum Amyloid A (SAA), plays a previously unknown key role in this vital process.
SAA has long been known to reroute lipid transport during inflammation, but the biological significance of this rerouting remained enigmatic. An important property of this protein is that its levels in blood increase rapidly and dramatically (over one thousand-fold) during an acute infection, injury, inflammation or after surgery. How does this dramatic but transient increase help the body to survive these acute events?
Now, researchers from Boston University School of Medicine (BUSM) have found that SAA plays several previously unknown roles in lipid transport necessary in cleaning up cell debris from the sites of injury. The studies were spearheaded by the corresponding author Shobini Jayaraman, PhD, senior scientist in the department of Physiology and Biophysics.
“Our study provides new insights into the key beneficial function of SAA that helps us survive injury, infection and inflammation. In other words, our study helps establish raison d’etre for this enigmatic ancient protein,” explained principal investigator Olga Gursky, PhD, professor of Physiology and Biophysics.
The researchers used recombinant SAA protein generated in the laboratory of Marcus Fändrich, professor and director of the Institute of Protein Biochemistry at Ulm University, Germany. The detailed biochemical analysis by Jayaraman found that SAA not only provided protein-lipid nanoparticles that are necessary for the lipid breakdown to proceed, but also helped remove its insoluble toxic products. Removal of such products is necessary to avoid their toxic effects. These in-vitro studies suggest a dual role for SAA in removing lipid debris from the dead cells in vivo.
According to the researchers, since SAA has been highly evolutionally conserved for at least 500 million years, it must have been beneficial for survival. “Our study proposes such a beneficial role and links SAA to another ancient acute-phase protein, secretory phospholipase A2 (sPLA2). Our results suggest that, together, SAA and sPLA2 act rapidly and efficiently to remove lipids from injured sites, which is necessary for tissue healing in vivo. We propose that this lipid removal helped diverse organisms to survive injury and infection throughout evolution.”
The researchers hope that this and other related studies will ultimately help better treatment of acute inflammation and may lead to better understand and, ultimately, alleviate chronic inflammation wherein SAA deposition in kidneys and other organs is a major life-threatening complication.
These findings appear online in the journal eLIFE.
Funding for this study was provided by National Institutes of Health grants GM067260, the Stewart Amyloidosis Endowment Fund, and the Deutsche Forschungsgemeinschaft grant FA456/15-1.