Unraveling Melanoma’s Mysteries
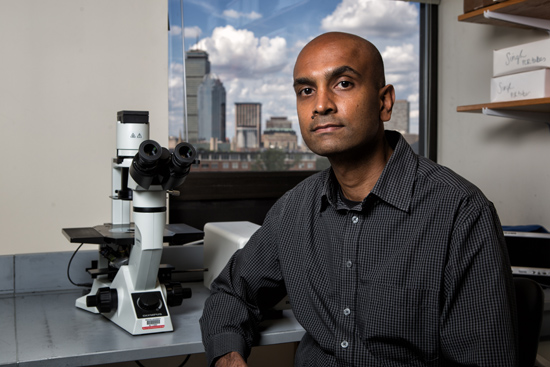
MED’s Anurag Singh wins grant to study gene in deadly skin cancer
Skin cancer is the most common of all cancers, with about 3.5 million cases diagnosed in the United States each year, according to the American Cancer Society. And while melanoma is one of the least common types, representing only about 2 percent of skin cancer cases, it is one of the most deadly. Melanoma is so aggressive that doctors measure the tumor depth under a microscope—the variance of a fraction of a millimeter may make the difference between survival and death.
Knowledge about this disease has taken off since 2002, when scientists discovered tumor-inducing mutations in the BRAF gene in over 50 percent of melanoma cases. Drugs that target mutant BRAF, along with new therapies that boost a patient’s immune system, have given doctors and patients hope, but treatments are still only partially effective. “Cancer is really smart,” says Rhoda M. Alani, the School of Medicine’s Herbert Mescon Professor and Chair of dermatology. “Patients respond to treatment, but then the cancer becomes resistant. We can make the cancer go away with targeted therapies, but it almost always comes back.”
In addition, says Alani, some forms of melanoma have no targeted therapy at all. About 20 percent of melanomas have a mutated gene called NRAS. These types of melanomas have no effective targeted treatment to date. That’s where Anurag Singh comes in.
Singh, a MED assistant professor of pharmacology and medicine, is tackling this poorly understood melanoma by investigating how NRAS transforms healthy, normal skin cells into aggressive cancerous cells. The work is funded by a three-year, $150,000 grant from the Melanoma Research Alliance.
RAS genes—named for “rat sarcoma” because that’s where scientists first found them—belong to a family of molecules called G proteins, which are important for much signaling within human cells. There are about 200 G proteins of various shapes and sizes, but they all have one thing in common: they can become activated and then, after some period of time, automatically turn themselves off.
Mutant forms of RAS have a problem: they can turn on, but they can’t turn off. The mutant RAS is always on, always signaling, even when other signals order it to cease and desist. This nonstop signaling can lead to different effects: sometimes it makes a cell multiply uncontrollably, sometimes it prevents a cancer cell from self-destructing. This makes the mutant forms of RAS common in cancer, but scientists still don’t know exactly how the mutations lead to disease.
“The RAS mutation itself is not sufficient to cause a full-blown tumor,” says Singh. “It creates a vulnerable state that can progress to a malignant state.”
Singh’s lab studies how two forms of the RAS gene, NRAS and KRAS, interact and cooperate with other genes to form gene networks, analogous to computer circuits. The RAS mutations prevalent in melanoma also appear in pancreatic and colon cancer. Singh has already discovered that melanomas with NRAS mutations come in at least two different flavors. “We have identified two major types of NRAS networks in melanoma,” he says. “We hypothesize that these subtypes can be treated with selective targeted anticancer agents or precision medicines. We hope to pinpoint vulnerabilities that can be blocked with chemotherapy.”
“Singh’s work is fundamental, basic science, but he has a strong interest in translational research,” says Alani. “It’s important to collaborate with physicians and think about specific applications, especially at a research institution like MED.”
While much of Singh’s work looks at signals within an individual cell, he’s also interested in how cells communicate with each other. “I’d like to study how an oncogene such as RAS regulates the tumor’s microenvironment, and how that might affect interactions with the surrounding cells,” he says. This network communications map could provide valuable clues to how cancers grow and survive, and how medicine might be able to fight them.
“That’s what I think about: how can we effectively treat patients with mutations in the RAS genes,” Singh says. “Ultimately, we’re all in the business of trying to advance therapeutics to benefit patients.”
This BU Today story was written by Barbara Moran. A version of this article originally appeared on BU Research.